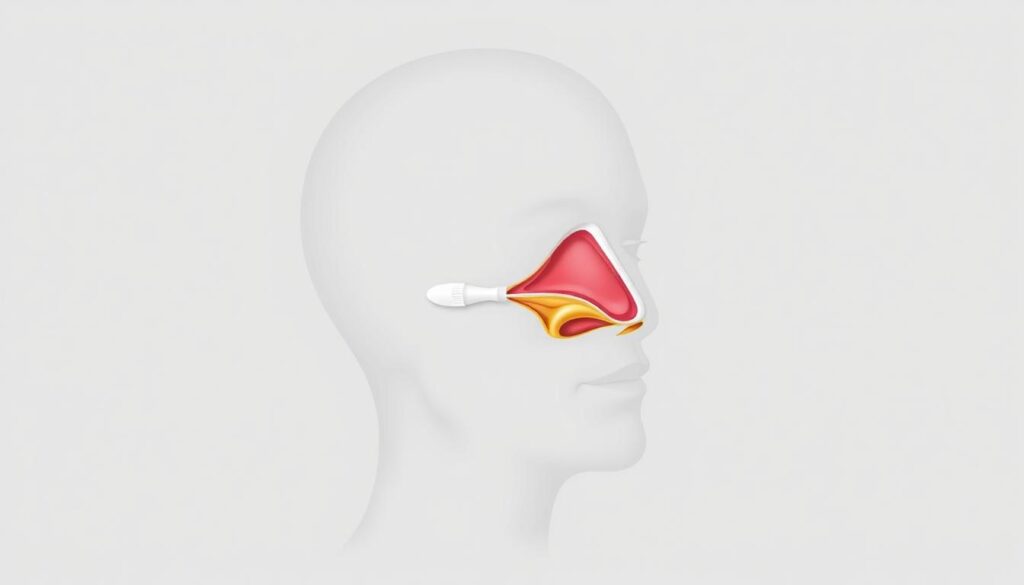
Could a small nasal problem be why you can’t sleep well? Many don’t know that up to 80% of us have a deviated septum. This is a crooked wall between the nostrils. But, could this small issue be linked to serious sleep problems like sleep apnea?
Worldwide, nearly a billion people have sleep apnea. In the U.S., 30 million have obstructive sleep apnea. The link between these two is important. Your nasal passages might seem far from breathing pauses at night. But, research shows deviated septums can narrow airflow, making snoring and sleep problems worse. Could fixing your septum help you sleep better?
Here’s the truth: a deviated septum alone doesn’t always cause sleep apnea. But, it can make symptoms worse. This article explores if your nasal structure might be causing poor sleep. And how to find relief. Let’s find out the facts before your next restless night.
Key Takeaways
- 80% of people have a deviated septum, often without knowing it.
- Snoring and sleep apnea might share a hidden link through nasal blockages.
- Chronic nasal congestion from a deviated septum could increase mouth breathing and worsen sleep quality.
- ENT specialists and sleep experts are studying how septum corrections affect sleep apnea outcomes.
- Over 30 million Americans with sleep apnea may benefit from understanding nasal anatomy’s role.
Understanding Deviated Septum: What It Means for Your Breathing
Your nasal septum is the wall that divides your nostrils. A deviated septum happens when this wall moves to one side. This makes breathing uneven. Surprisingly, nasal congestion from this issue affects 80% of people, but many don’t notice it.
What Exactly Is a Deviated Septum?
This shift can block airflow, causing difficulty breathing. While most cases are minor, severe deviations make breathing hard, especially at night. Imagine one nostril working harder than the other. This imbalance can get worse over time.
Common Causes of Septal Deviation
- Born with the condition (congenital)
- Nasal injuries from sports, accidents, or falls
- Natural aging that shifts cartilage
How to Recognize the Signs of a Deviated Septum
Common symptoms include:
- Unilateral nasal congestion (one nostril blocked more than the other)
- Chronic difficulty breathing through the nose
- Facial pain, frequent nosebleeds, or postnasal drip
- Noisy breathing or snoring at night
If these symptoms sound familiar, they could signal a deviated septum needing evaluation. Even mild cases may cause sleep disruptions. This can lead to bigger health problems later on.
Sleep Apnea Explained: More Than Just Snoring
Snoring might seem harmless, but sleep apnea is a serious sleep disorder. It stops your breathing dozens—even hundreds—of times each night. This condition disrupts your sleep cycle, leaving you feeling exhausted despite spending hours in bed.

Obstructive sleep apnea (OSA) is the most common form, affecting around 30 million Americans. It happens when throat muscles relax too much, narrowing or closing your airway. This blockage causes gasping or choking sounds, not just loud snoring. Without treatment, OSA raises risks for high blood pressure, heart disease, type 2 diabetes, and weakened immunity.
Many people with OSA don’t realize they have it. Symptoms like morning headaches, daytime sleepiness, or waking up gasping are easy to ignore. Yet, untreated sleep apnea harms your health over time. Here’s why it matters:
- Repeated breathing pauses strain your heart and lungs
- Chronic fatigue weakens focus and mood
- Long-term risks include metabolic and cardiovascular diseases
If you suspect sleep apnea, talk to a doctor. Early diagnosis can prevent serious complications and improve your quality of life. Don’t let silence about snoring cost your health.
Can a Deviated Septum Cause Sleep Apnea? The Scientific Connection
Understanding how your nasal health impacts sleep starts with the basics. A deviated septum doesn’t directly cause sleep apnea. But it can make symptoms like nasal congestion and snoring worse. Let’s explore the science behind this complex relationship.

The Airflow Problem: How Nasal Obstruction Affects Sleep
Your nasal passages protect you from airway blockages. A deviated septum narrows these passages. This forces you to breathe through your mouth.
This change affects air pressure in your throat. It makes it harder to keep your airway open. Mouth breathing can make snoring worse and increase breathing pauses. Chronic nasal congestion also strains your airways, especially during sleep.
Research Evidence on the Relationship
“The study found that individuals with a deviated septum were 4.39 times more likely to develop sleep apnea than those without the condition.”
- The study followed 33,714 people for 9 years. It found 22.41 sleep apnea cases per 10,000 in the deviated septum group. Healthy individuals had 5.12 cases.
- Risk increases with obesity. Those with Class III obesity (BMI ≥40) faced 197.2x higher risk when combined with a deviated septum.
Risk Factors That Strengthen the Connection
Your lifestyle and anatomy play a big role. These factors increase the chance of sleep apnea with a deviated septum:
- High BMI: Overweight patients see risk multipliers of 3–197x depending on obesity class.
- Age: Under-50 patients had a 21% higher risk compared to older groups.
- Diabetes: Patients with diabetes faced a 2.44x higher risk of OSA.
Surgery like septoplasty improves breathing. But it doesn’t eliminate sleep apnea entirely. Combining treatments like CPAP adjustments and nasal steroids often yields better results.
Symptoms That Suggest Both Conditions May Be Present

Do you notice patterns in how you feel during the day or night? Certain symptoms could mean you have a sleep disorder related to both a deviated septum and sleep apnea. These signs often overlap, making early recognition key for treatment.
Daytime Signs to Watch For
| Symptom | Prevalence |
|---|---|
| Difficulty breathing through one nostril | Common in severe cases (20% of those affected) |
| Unshakable daytime sleepiness | Linked to untreated sleep apnea |
| Nasal congestion or stuffiness | Affects most symptomatic individuals |
| Mood changes or irritability | Reported in 30-50% of cases |
Nighttime Symptoms That Shouldn’t Be Ignored
- Loud, persistent snoring (affects 40% of deviated septum patients)
- Witnessed breathing pauses during sleep
- Gasping or choking while asleep
- Severe difficulty breathing that disrupts sleep
- Chronic snoring accompanied by gasping
- Daytime fatigue impacting work or daily tasks
- Headaches or facial pain (10-15% report this)
When to Seek Medical Attention
Visit a specialist if you experience:
Early action is crucial. These symptoms can get worse over time if not treated. Make your health a priority by seeing an ear, nose, and throat (ENT) specialist for a proper check-up.
Diagnosing Your Condition: What to Expect at the Doctor’s Office

Your doctor will first look at your nose for a deviated septum. They’ll use a light and a tool called a nasal speculum. This helps them see if there are any problems.
If they think you might have sleep apnea, they might ask you to do a sleep study. This study watches your breathing and oxygen levels when you’re sleeping.
- Physical Exam: A quick check of your nasal passages to identify a deviated septum.
- Sleep Study: Measures breathing patterns, oxygen levels, and snoring activity to confirm sleep apnea.
- Additional Tests: Imaging scans or questionnaires help assess how these issues affect your sleep quality.
| Test | Purpose | Details |
|---|---|---|
| Nasal Exam | Check for septum deviation | Performed in-office; takes 5-10 minutes |
| Polysomnography | Diagnose sleep apnea | Overnight lab test tracking brain waves, breathing, and heart rate |
| Home Test | Screen for sleep apnea | Use sensors to track blood oxygen and airflow in your own bed |
Over 80% of people have some nasal blockage from a deviated septum, but not all need surgery.
Getting accurate results is very important. They help your doctor figure out the best treatment. This could be surgery for the septum or devices for sleep disorder management.
Don’t be shy to ask questions. Knowing what comes next and how it relates to your symptoms is key. Early diagnosis can really help improve your breathing and sleep quality.
Treatment Options for Deviated Septum When Sleep Apnea Is Present
If your deviated septum causes sleep apnea or breathing problems, there are ways to help. Some people don’t need treatment for mild cases. But, severe cases might need more help. Let’s look at options that might work for you.
Try simple steps first to see if they help. You might use:
- Nasal strips to widen airways temporarily
- Steroid nasal sprays to reduce inflammation
- Antihistamines or decongestants for allergy-related swelling
These can help for a little while. But, they might not fix the problem for good. Talk to your doctor to see what’s best for you.
Septoplasty is a surgery to fix breathing problems. It’s done to help you breathe better, not to change how you look. It’s usually done as an outpatient procedure.
It’s for people with big problems like sleep apnea or infections. You’ll feel better in a few weeks. You might breathe easier and snore less.
After surgery, you’ll rest a bit in a recovery room. Then, you go home. Swelling goes down in a few days. It takes weeks to fully heal.
Most people breathe better and sleep better at night. But, sleep apnea might still need extra help like CPAP therapy. Talk to your surgeon about what you can expect.
Managing Sleep Apnea When You Have a Deviated Septum
Nearly 70% of people with sleep apnea have nasal blockages. This is often due to a deviated septum. Your doctor might suggest using treatment options for both problems. Here’s how to find the right care for your unique needs:
- CPAP Therapy: Machines like CPAP or BiPAP devices push air through a mask. This keeps airways open. You might need nasal pillows or full-face masks.
- Oral Appliances: Custom mouth guards reposition your jaw. This reduces airway blockages during sleep.
- Surgery: Septoplasty fixes the septum, and UPPP surgery tightens throat tissues. Studies show combining both can reduce obstructive sleep apnea by 70%.
- Lifestyle Adjustments: Nasal sprays, weight loss, and avoiding back-sleeping can help.

| Treatment | How It Works | Pros | Cons |
|---|---|---|---|
| CPAP | Uses mild air pressure to keep airways open | Effective for severe cases | Mask discomfort |
| Oral Appliances | Adjust jaw position to clear the airway | Portable | May not suit severe cases |
| Surgery | Corrects structural nasal issues | Long-term relief | Recovery time |
“Combined surgery and CPAP use improved sleep quality in 80% of participants.”
Work with your team to find the best treatment options. For example, a deviated septum might need a full-face CPAP mask. Regular check-ups help adjust your plan as needed. Even small changes, like using a humidifier or nasal strips, can help.
Lifestyle Changes That Can Improve Both Conditions
Small changes in daily habits can greatly help with sleep apnea and nasal congestion. Let’s look at easy steps to breathe better and sleep well.

Sleep Position Adjustments
Sleeping on your side can cut down on snoring and improve airflow. Here are some tips:
- Place a pillow between your knees or behind your back to stay on your side.
- Use a positional alert device that vibrates if you roll onto your back.
Dietary and Exercise Considerations
Extra weight puts pressure on airways. Losing 10% of your weight can reduce sleep apnea symptoms by half. Avoid alcohol and sedatives before bed as they relax throat muscles and make snoring worse. A study showed that diet changes and exercise helped one patient lose 50 pounds, ending their need for CPAP therapy.
After losing weight and adjusting my sleep habits, I stopped using my CPAP and felt rested for the first time in years.
Optimal Sleep Environment
Create a calm space for better sleep:
- Use a humidifier to reduce nasal dryness and congestion.
- Raise your head with pillows to ease airflow.
- Keep the room dark and cool to improve sleep quality.
Small changes like these can help reduce snoring and improve your overall sleep health.
Success Stories: How Treating a Deviated Septum Improved Sleep Apnea
Real people’s stories show how fixing a deviated septum can change sleep for the better. While can a deviated septum cause sleep apnea isn’t a clear yes, fixing nasal blockages often helps. Here are some outcomes:

“After septoplasty, I finally breathe through my nose at night. My CPAP machine is a backup now—my sleep apnea episodes dropped by half.” — Sarah, 38
Many patients find relief through treatment options like surgery. Studies show 70–80% see better airflow. Here’s what changes look like:
- Some see full resolution of sleep apnea symptoms after surgery.
- Others use CPAP at lower pressure settings post-septoplasty.
- Combined approaches (surgery + lifestyle changes) boost results for many.
Take Mark, 52: his difficulty breathing at night vanished. “I stopped gasping for air during sleep. My wife says I stopped snoring entirely,” he shared. Yet results vary. Some need follow-up care, like nasal sprays or continued CPAP use.
Septoplasty isn’t a cure-all. Risks include temporary swelling or recurrence, but most patients report better sleep and energy. Recovery takes weeks, but long-term benefits often outweigh minor downsides.
If you’re weighing options, remember: surgery addresses the root cause of nasal blockage. Talk to a specialist to see if correcting your septum could be your first step toward better rest.
When to Consider Combined Treatments for Both Conditions
Managing a deviated septum and obstructive sleep apnea needs a team effort. If CPAP machines don’t help with difficulty breathing at night, try combining treatments. Surgery for a deviated septum might make CPAP therapy work better.
Coordinating Care Between Specialists
Work with three key experts:
- ENT (ear, nose, and throat) doctors to address structural nasal issues
- Sleep specialists to monitor obstructive sleep apnea severity
- Primary care providers to track overall health impacts
Ask for shared records and written treatment plans. This ensures all specialists are working towards the same goals.

Insurance and Cost Considerations
Most insurance plans cover sleep studies or surgeries. But, check the details first:
- See if septoplasty and CPAP devices are medically necessary
- Find out about annual deductibles for surgery costs
- Look into payment plans for any out-of-pocket costs
Keep records of how nasal blockages affect your sleep apnea. This helps prove medical necessity.
Conclusion: Taking Control of Your Breathing and Sleep Health
If you’ve wondered, “Can a deviated septum cause sleep apnea?” you now know the answer is complex. A deviated septum alone doesn’t directly cause sleep apnea. But, it can make breathing problems worse, making sleep disorders harder to handle.
If you snore, feel tired during the day, or have trouble breathing through your nose, see a specialist. Early diagnosis is crucial. It helps find the right treatment for you.
Veterans with sleep apnea linked to nasal problems might get higher VA disability ratings. Programs like Claims Insider have helped thousands get better compensation. They’ve even increased ratings by 10 or more points.
If your claim was denied before, reviewing it could help you get the support you need. A deviated septum is a common condition. It’s important for healthcare providers to focus on it.
Treatment options like septoplasty can greatly improve your life. Studies show patients can smell better after surgery. Younger patients also see their blood pressure drop.
Combining surgery with lifestyle changes, like using CPAP machines or adjusting sleep positions, can help. Remember, symptoms like chronic headaches and daytime sleepiness are not normal. Getting help early can prevent serious health problems.
Taking control starts with talking openly with your doctor. There are many options to ease symptoms. Sleep health affects every part of your life, from work to relationships. Don’t hesitate to explore all options for your well-being.