Ever thought a stuffy nose and sinus pressure could cause snoring or restless nights? The link between sinus infections and sleep apnea is interesting. With 31% of adults getting sinusitis each year, and 40% of sleep apnea patients also having sinus issues, it’s not just a coincidence.
Let’s look into how sinus problems and sleep issues are connected. And what it means for your health.
Key Takeaways
- Over 12% of U.S. adults have chronic sinusitis, often paired with sleep apnea symptoms.
- Nasal congestion from sinus infections can reduce airflow by 20%, worsening breathing at night.
- Up to 60% of chronic sinusitis patients report sleep disturbances like snoring or apnea episodes.
- Combined treatment for both conditions improves sleep quality by up to 50% in many cases.
- Chronic inflammation from sinusitis may increase sleep apnea risk by 2-3 times.
Understanding Sinus Infections and Their Symptoms
Sinus infections, or sinusitis, can really mess up your day and sleep. Both sinus infection and sleep apnea have similar symptoms like a stuffy nose. It’s important to know how these conditions affect each other.
Common Signs of Acute Sinusitis
Acute sinusitis usually lasts less than four weeks. Here are some signs to watch for:
- Facial pain or pressure around eyes, cheeks, or forehead
- Thick yellow/green mucus discharge
- Stuffy nose that makes it hard to breathe
- Headaches, fatigue, or loss of smell
Chronic Sinusitis and Its Effects
If symptoms last more than 12 weeks, you might have chronic sinusitis. This affects over 10 million Americans and can make sinusitis and sleep apnea symptoms worse. Chronic inflammation can:
- Make it hard to sleep: 64% of chronic sufferers have trouble breathing at night
- Make you feel tired: Constant congestion makes it hard to rest
- Affect your mind: Chronic sinusitis patients score 25% lower on cognitive tests than healthy people
Chronic sinusitis patients reported 60 billion USD in annual healthcare costs. This shows the big physical and financial impact of not treating it.
Risk Factors for Developing Sinus Infections
Some people are more at risk because of:
- Anatomical issues (deviated septum, narrow sinus passages)
- Allergies or asthma causing nasal swelling
- Weakened immunity from diabetes or smoking
- Long-term exposure to pollution or secondhand smoke
Allergies can increase your risk of sleep-disordered breathing by 80%. Knowing these risk factors can help prevent problems like obstructive sleep apnea.
What Is Sleep Apnea and Who Is at Risk?
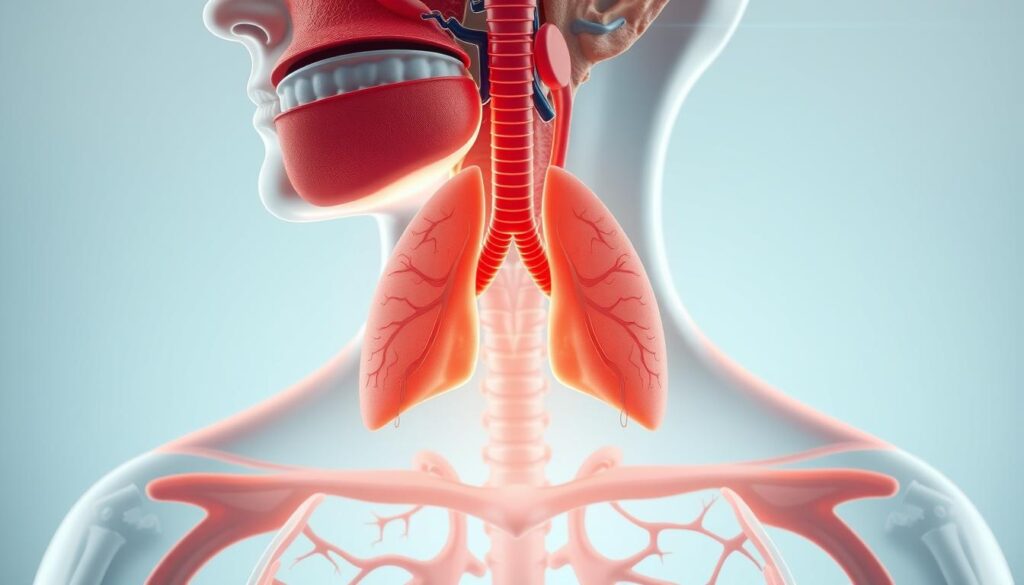
Sleep apnea makes breathing stop during sleep. This can happen for seconds or minutes. Obstructive sleep apnea (OSA) is when your throat muscles relax too much. This blocks the airway.
Imagine waking up hundreds of times a night. You might not even know it. This breaks your deep sleep.
Signs include loud snoring, gasping for air, morning headaches, and feeling tired all day. Feeling very tired, even after sleeping a lot, could be a sign. Here are some groups at higher risk:
- Weight: More than 70% of OSA cases are linked to being overweight. This is because extra fat can narrow your airways.
- Gender: Men are 2–3 times more likely to get OSA before menopause than women.
- Nasal issues: Problems like sinus infections or chronic congestion can make breathing harder. This can make sleep apnea symptoms worse. Chronic sinusitis can increase your risk of OSA by up to 30%.
- Age: The risk of OSA goes up after 40, especially in your 50s-60s.
The impact of sinus infection on sleep apnea is clear. Swollen sinuses can block the airway. This creates a cycle where sinus problems and sleep apnea are linked. For example, people with chronic sinusitis often have worse snoring and feel more tired during the day.
A 2023 study found 40% of people with chronic sinusitis also had OSA. This shows how dangerous this connection is.
| Risk Factor | Impact |
|---|---|
| Obesity | Increases airway blockage risk |
| Smoking | Inflames airways, worsening breathing |
| Sinusitis | Directly contributes to nasal obstruction |
If you often get sinus infections or notice symptoms like constant snoring, see a doctor. Early treatment can stop serious health problems like heart disease or diabetes.
Can Sinus Infection Cause Sleep Apnea?
Sinus infections and sleep apnea are closely linked. Swollen nasal passages from sinusitis block airflow. This forces you to breathe through your mouth.
This change disrupts normal breathing patterns. It increases your risk of sleep apnea episodes. Let’s explore how this happens.
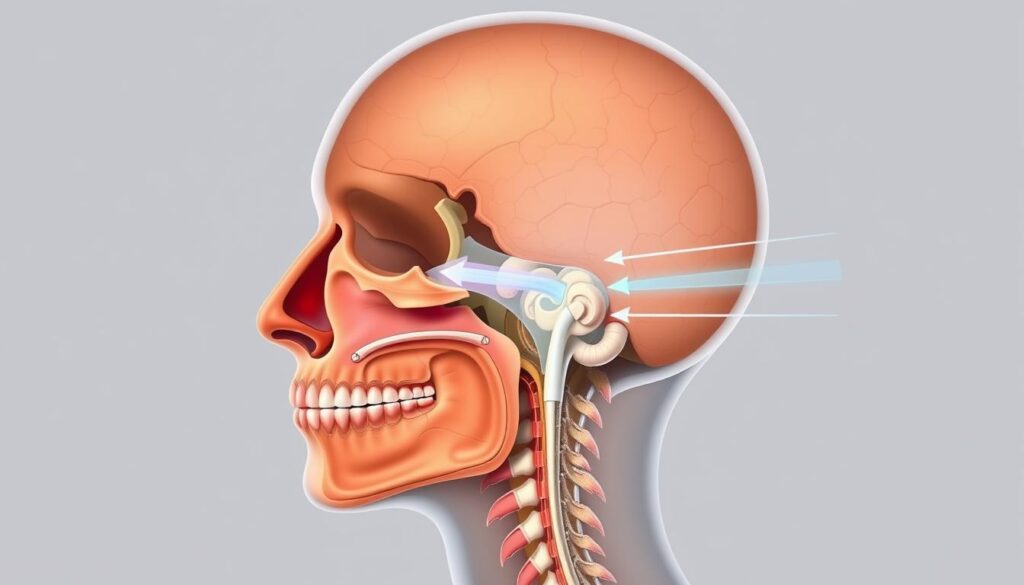
The Physiological Connection
When sinus tissues swell, nasal blockage occurs. Here’s how it progresses:
- Inflamed sinuses reduce airflow through the nose
- Mouth breathing creates unstable air pressure in the throat
- Unstable air pressure pulls soft tissues inward, blocking the airway
| Sinus Issues | Sleep Apnea Symptoms |
|---|---|
| Facial pressure/pain | Gasping for air during sleep |
| Thick mucus buildup | Choking sensations |
| Nasal congestion | Daytime fatigue |
Research Evidence Supporting the Link
A study of 971 sleep apnea patients found many had sinus issues before. Dr. Papgianopolous found untreated sinusitis raises sleep apnea risk by 30%. These studies show the two often go together.
“Chronic sinus inflammation creates a cycle where each condition worsens the other.”
When Temporary Sinus Issues Lead to Sleep Disorders
Even short-term sinus infections can have lasting effects. Persistent congestion makes your body rely on mouth breathing. This changes your breathing patterns over time.
This increases your risk of chronic sleep apnea. Treating sinus issues early can prevent this.
If you often have sinus problems, see your doctor. They might suggest nasal irrigation or saline sprays. Early treatment can lower your risk of sleep problems.
Consider balloon sinus dilation or other treatments. They can help restore normal airflow before it becomes permanent.
How Nasal Congestion Affects Your Breathing During Sleep
Nasal congestion from sinus infections messes with your sleep. The relationship between sinusitis and sleep apnea is clear when you can’t breathe through your nose. This makes you breathe through your mouth, disrupting your sleep.
Studies show lying down makes breathing harder. Nasal resistance can increase by up to 0.20 Pas/cm³. This makes it tough to breathe well.

The Impact of Blocked Airways on Sleep Quality
When sinuses are inflamed, airways narrow. This starts a cycle:
- Low oxygen leads to sleep cycle breaks
- Chronic sinusitis patients often gasp at night
- Severe cases have nasal resistance over 0.80 Pas/cm³, meeting medical criteria
This messes up deep, restorative sleep. You might feel tired even after 8 hours.
Mouth Breathing and Its Consequences
Forced mouth breathing skips your nose’s natural filters. This causes:
- Dry, irritated throat tissues
- More intense snoring
- Soft palate vibrations that worsen sleep apnea episodes
Research shows sleeping on your side can reduce nasal resistance by up to 50%. This pattern can change your airways over time. It makes the sinus infection and sleep apnea connection more dangerous.
Distinguishing Between Sinus-Related Sleep Issues and True Sleep Apnea
It can be hard to tell if your sleep problems come from sinus issues and sleep apnea or sinusitis and sleep apnea. Both can mess with your sleep, but they have different causes and treatments. Sinus infections cause short-term symptoms like facial pressure and thick mucus. Sleep apnea, on the other hand, means your airway blocks many times during the night.
A 2016 study found important information. It showed that people with obstructive sleep apnea (OSA) had 6.59% rates of chronic sinusitis. This is compared to just 2% in those without OSA. This shows a link, but not a direct cause. If your breathing problems go away after treating your sinuses, it’s likely due to inflammation. But if snoring and gasping keep happening, it could be apnea.

- Sinus-related disruptions usually improve within 8 weeks with antibiotics or nasal sprays.
- Apnea symptoms remain even after sinus treatment, often linked to throat muscle collapse.
- Daytime fatigue from sinusitis fades as congestion clears. Apnea-related tiredness lingers without CPAP therapy.
Doctors use CT scans to check sinus swelling and sleep studies to track breathing patterns. If your symptoms stick around after antibiotics or nasal decongestants, a sleep study might be next. Early diagnosis is key—untreated apnea raises risks for heart disease and diabetes. Sinusitis left untreated can lead to infections spreading.
Ask your doctor about imaging tests if you’re unsure. Remember: temporary nasal congestion points to sinusitis, but persistent gasping for air means it’s time to explore apnea evaluations. Your health depends on knowing the difference.
The Relationship Between Sinusitis and Sleep Apnea
Understanding the relationship between sinusitis and sleep apnea shows a cycle. Each condition can make the other worse. Let’s look at how to manage both well.

How Chronic Sinusitis Worsens Existing Sleep Apnea
Chronic sinusitis makes nasal passages narrower. This increases airway resistance, especially for sleep apnea. Symptoms like snoring and oxygen drops during sleep get worse.
Chronic inflammation from sinus infections also thickens mucus. This blocks airflow even more.
- Inflamed sinuses trap mucus, reducing nasal airflow
- Swelling from sinusitis can collapse airways during sleep
- Untreated sinus infections delay sleep apnea treatment effectiveness
When Sleep Apnea Contributes to Sinus Problems
Sleep apnea’s oxygen changes can lead to connection between sinus infection and sleep apnea. Low oxygen during pauses triggers sinus inflammation. This creates a cycle. Here’s what research shows:
| Group | Sinusitis Risk | Study Period |
|---|---|---|
| Sleep Apnea Patients | 7% developed sinusitis | 5 years |
| Non-Sleep Apnea Group | 2% developed sinusitis | 5 years |
Breaking the Cycle of Mutual Aggravation
To break this cycle, treat both conditions at the same time. Try these steps:
- Use CPAP therapy to keep airways open nighty
- Hydrate daily to thin mucus and reduce congestion
- Use saline rinses to clear nasal passages before bed
- Avoid alcohol and allergens that trigger inflammation
Regular visits to an ENT specialist are key. They help spot when sinus issues or sleep apnea get worse. Small changes can greatly improve your situation.
Diagnosing Sinus Problems and Sleep Disorders
Getting the right diagnosis is key to breaking the cycle of sinus problems leading to sleep apnea. Start by seeing an ENT specialist or sleep medicine doctor. They’ll check for sinus blockages using tools like CT scans or nasal endoscopy to spot inflammation or polyps. Sleep specialists may recommend overnight sleep studies to measure breathing patterns and oxygen levels.

- Physical exams to assess nasal swelling or drainage
- Imaging scans like CTs to map sinus structure
- Overnight sleep studies (polysomnography) to track apnea events
- Allergy tests if environmental triggers are suspected
Data shows 64% of chronic sinusitis patients have clinically significant sleep apnea. The impact of sinus infection on sleep apnea is clear: higher PSQI scores (average 9.4) and daytime sleepiness (EpSS scores over 10) are common in sinus sufferers. A Utah study found CRS patients scored 38% worse on cognitive function tests than healthy peers.
Don’t delay care. Early diagnosis prevents complications like heart strain or daytime fatigue. Your doctor might recommend allergy shots, nasal steroid sprays, or CPAP machines to address both conditions. Remember, proper testing ensures you get the right treatment—not just for snoring, but for long-term health.
Treatment Options That Address Both Conditions
Managing sinusitis and sleep apnea together can break the cycle of mutual aggravation. Treating sinusitis to improve sleep apnea often requires a mix of therapies targeting both systems. Let’s explore options that address both conditions effectively.

Medical Interventions for Sinus Infections
Start with treatments that reduce sinus inflammation and drainage:
- Antibiotics like amoxicillin or azithromycin for bacterial infections.
- Nasal corticosteroids (e.g., fluticasone) to shrink swollen tissue.
- Saltwater irrigation to clear mucus and reduce pressure.
Culture-directed antibiotics ensure you get the right drug for your infection. This helps address sinus problems leading to sleep apnea at the source.
Sleep Apnea Therapies That Help Sinus Symptoms
Devices like CPAP machines improve airflow and nasal health:
- CPAP therapy delivers steady air pressure, easing congestion and keeping airways open.
- EPAP devices (e.g., Provent) reduce OSA symptoms by 53% while easing nasal blockages.
- Zepbound (setmelanched), approved by the FDA, helps obese patients lose weight. This eases both sinus and sleep issues.
When Surgery Might Be Necessary
Severe cases may require procedures to permanently open airways. Here’s what to expect:
| Surgery | Goal | Success Rate |
|---|---|---|
| Functional endoscopic sinus surgery (FESS) | Unclog sinus passages | Reduces symptoms in 80% of patients |
| Uvulopalatopharyngoplasty (UPPP) | Remove obstructive tissue | Up to 50% effective for OSA |
| Maxillomandibular advancement | Expand the airway | 87% symptom reduction |
Combining therapies tailored to your needs offers the best chance for relief. Always consult a doctor to create a plan that works for you.
Lifestyle Changes to Improve Sinus Health and Sleep Quality
Making small changes in your daily life can greatly help. These steps can improve both treatment options for sinusitis and sleep apnea. They help by addressing the impact of sinus infection on sleep apnea in simple ways.

Environmental Modifications for Better Breathing
Here are some tips for a cleaner sleep area:
- Use air purifiers to remove allergens like dust mites, which cause 70% of sleep apnea cases linked to nasal blockage.
- Keep humidity between 40-50% to prevent dry air from worsening congestion.
- Wash bedding weekly in hot water to eliminate allergens—treating sinusitis to improve sleep apnea starts with a clean space.
Dietary Considerations for Reducing Inflammation
Your diet can affect your airways. Focus on:
| Anti-Inflammatory Foods | What to Avoid |
|---|---|
| Fatty fish (salmon), turmeric, leafy greens | Processed foods, alcohol (linked to 25% higher apnea risk) |
| Water to thin mucus | Caffeine before bed (disrupts sleep cycles) |
Sleep Position Adjustments for Optimal Airflow
Try these changes to help breathing:
- Sleep on your side to reduce airway collapse risk by 40%.
- Raise your head with a wedge pillow to prevent mucus pooling.
- Avoid (back sleeping) to cut snoring linked to sinus congestion.
70% of people see sleep improvements after adopting these changes!
Small steps can help break the cycle of sinus and sleep issues. If self-care isn’t enough, talk to an ENT specialist for a personalized plan.
Conclusion: Taking Control of Your Sinus Health and Sleep
Your sinuses and sleep are closely linked. The question can sinus infection cause sleep apnea is yes. Chronic sinusitis can make sleep apnea symptoms worse by blocking airways. Studies show people with chronic sinus issues are 75% more likely to have sleep problems.
But the relationship between sinusitis and sleep apnea goes both ways. Sleep apnea can also hurt your sinuses, making symptoms worse. This creates a cycle of worsening symptoms.
Understanding this connection is crucial for finding relief. If you have nasal congestion or frequent sinus infections, see a healthcare provider. They can suggest treatments like saline rinses, CPAP therapy, or surgery.
A 2015 study found sinus surgery helped many patients with both conditions sleep better. Lifestyle changes like using humidifiers or managing allergies also help.
With 1 billion people worldwide affected by obstructive sleep apnea, taking action is crucial. Simple steps like cleaning nasal passages with a neti pot or adjusting sleep positions can help. If issues persist, you might need prescription drugs or a CPAP machine.
Remember, untreated sleep apnea can increase risks for heart disease and diabetes. So, addressing both sinus and sleep health is important for your long-term well-being.
Take charge of your health by recognizing these connections. Whether through over-the-counter decongestants, nasal strips, or professional care, there’s a path forward. Prioritize your breathing and sleep—your body and mind will thank you.