Ever had a stuffy nose or snored a lot? You might wonder if sinus trouble leads to sleep apnea. Millions in the U.S. deal with both, but the link isn’t always clear. Studies show a complex relationship between sinusitis and sleep apnea.
A five-year study in Scientific Reports followed 971 sleep apnea patients. It found only 7% later had sinusitis. This is lower than the 2% without sleep apnea. Yet, untreated chronic sinusitis affects over 30 million Americans. It can make breathing problems worse at night.
Sleep apnea blocks your throat, while sinusitis clogs your nasal passages. Both can disrupt sleep. But does one really cause the other? With millions of Americans affected, understanding this link could help you breathe better. Learn how sinus inflammation, congestion, and treatments like balloon sinuplasty might help bridge the gap.
Key Takeaways
- Over 30 million Americans have chronic sinusitis, a condition linked to sleep disruptions.
- Scientific Reports found no strong sinusitis and sleep apnea link in long-term data.
- Untreated sinusitis may raise sleep apnea risk by blocking airways during sleep.
- Both conditions share symptoms like snoring and breathing interruptions.
- Medical procedures like balloon sinuplasty address nasal blockages tied to both issues.
Understanding Sinusitis and Its Symptoms
Sinusitis is when the sinuses get inflamed. This makes breathing hard and can mess with sleep. It’s linked to sinus inflammation sleep apnea connection because blocked noses can make breathing at night worse.
What Exactly Is Sinusitis?
The sinuses’ lining swelling leads to mucus buildup. This causes pressure and congestion. About 12% of U.S. adults have chronic cases, leading to breathing problems.
For many, this inflammation makes sleep apnea symptoms worse. This is especially true when lying down at night.
Common Symptoms of Sinus Inflammation
Key signs include:
- Facial pain around the eyes, cheeks, or forehead
- Thick yellow or green nasal discharge
- Loss of smell or taste
- Headaches and fatigue
Nighttime symptoms like congestion get worse. This makes it hard to breathe through the nose. It can disrupt sleep patterns, leading to sleep apnea episodes.
Acute vs. Chronic Sinusitis
Acute cases last up to 4 weeks, often caused by colds or allergies. Chronic cases last more than 12 weeks, with symptoms like constant congestion and facial pressure.
Chronic cases affect sleep more, as ongoing inflammation narrows airways. This makes nighttime breathing worse. Studies show 30% of chronic sufferers have sleep apnea symptoms, showing the sinusitis symptoms worsen sleep apnea link.
What Is Sleep Apnea and Who’s at Risk?
Sleep apnea makes you stop breathing while you sleep. This can wake you up. It’s a big health problem. Here’s what you need to know.
Types of Sleep Apnea
There are three main types:
- Obstructive sleep apnea (OSA): Blocked airways, often from relaxed throat muscles or nasal congestion.
- Central sleep apnea: Your brain doesn’t tell muscles to breathe, less common but serious.
- Complex sleep apnea: A mix of OSA and central sleep apnea symptoms.

Risk Factors for Developing Sleep Apnea
Your risk goes up if you:
- Have a high BMI or a thicker neck.
- Are male, over 40, or have a family history.
- Smoke, drink alcohol, or use sedatives.
- Deal with nasal congestion or sinus issues linked to sleep apnea correlation. The relationship between sinusitis and sleep apnea becomes clear when sinus inflammation blocks airflow, worsening breathing interruptions.
Recent studies show 70% of OSA patients have nasal blockages, and 82.5% of those with rhino-sinus conditions face severe nasal obstruction.
How Sleep Apnea Affects Your Daily Life
Imagine waking up gasping for air many times a night. Daytime fatigue, headaches, and irritability are common. Untreated apnea raises risks for heart disease and stroke. For those with sinusitis, the sinus issues and sleep apnea correlation means congestion from sinus infections can worsen symptoms, creating a cycle of poor sleep and health strain.
Can Sinusitis Cause Sleep Apnea? Exploring the Connection

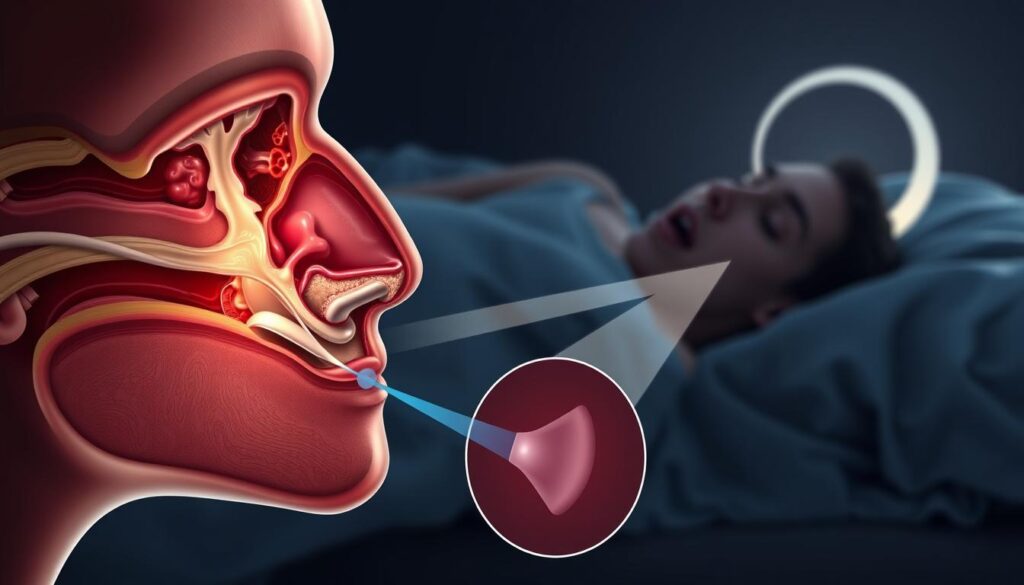
Does can sinusitis cause sleep apnea have a direct link? Research shows sinusitis doesn’t cause sleep apnea. But, it makes breathing harder. Sinus congestion makes your nose narrower, leading to mouth breathing.
This change in breathing can cause airway collapse during sleep. This is a big risk for sleep apnea.
| Condition | OSA Patients | Non-OSA Group |
|---|---|---|
| Chronic Sinusitis Cases | 64 (6.59%) | 97 (2.00%) |
| Hazard Ratio for CRS | 3.18 (adjusted) | — |
Studies of 5,826 patients show a strong link. Those with obstructive sleep apnea are 3.18 times more likely to get chronic sinusitis. Sinus congestion and sleep apnea affect each other.
Sinus congestion can strain your airways. Sleep apnea can make sinuses inflamed. This creates a cycle of problems.
- Chronic congestion forces mouth breathing, destabilizing airways
- Inflamed sinuses thicken nasal tissues, reducing airflow
- 64% of participants in UK studies reported worsened sleep due to sinus issues
A block quote from the study says: “Untreated chronic sinus infections significantly increase sleep apnea risks.” Even mild sinusitis can lead to sleep disorders if not treated.
Talk to your doctor if you have ongoing congestion. Early treatment can prevent heart disease and high blood pressure linked to both conditions.
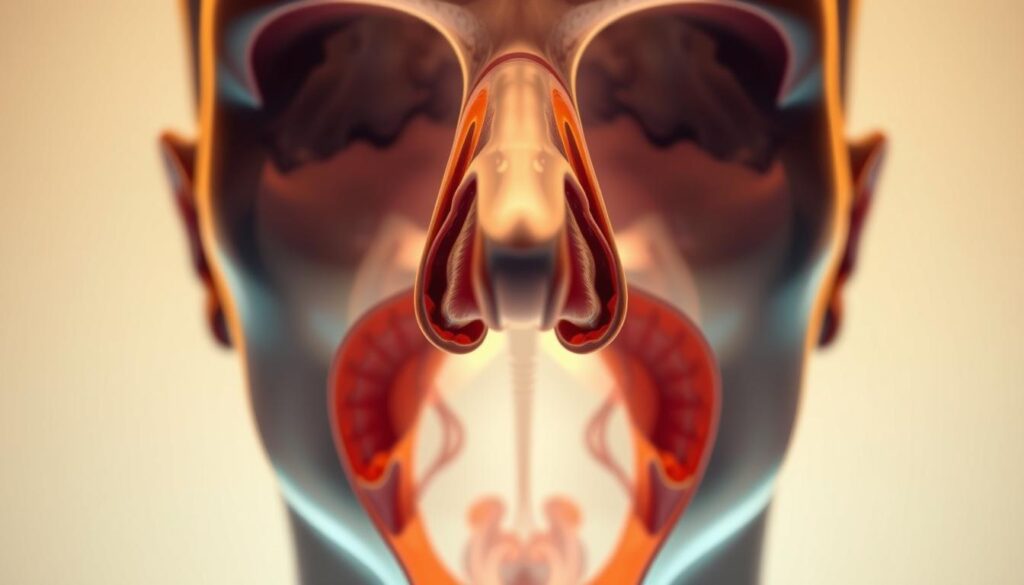
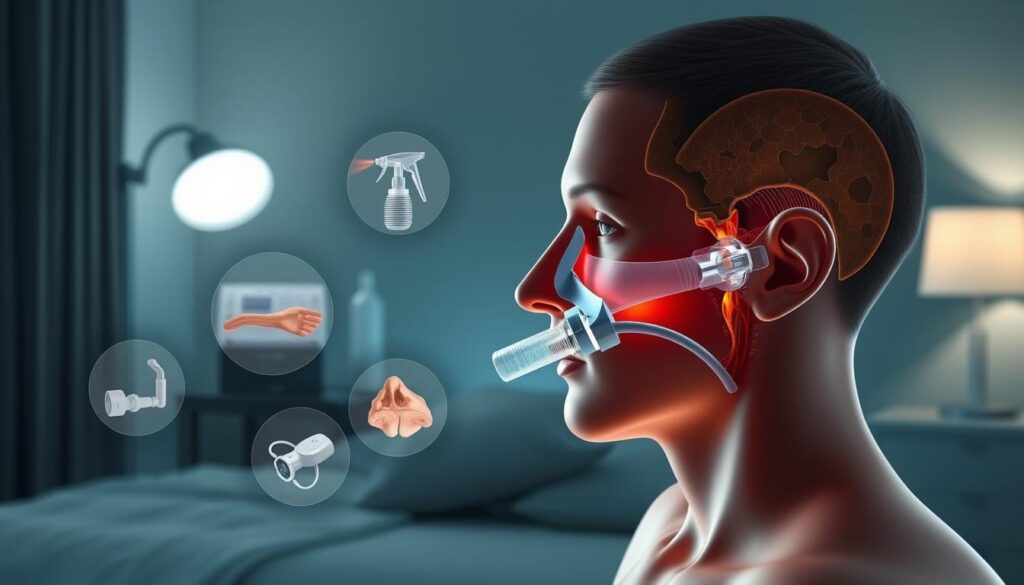
The Nasal Passageway’s Role in Breathing During Sleep
Your nose is more than just for smelling. It’s your body’s first line of defense at night. It makes sure air is filtered, warmed, and moistened. This keeps your airway open, stopping it from collapsing and disrupting sleep.
But sinusitis can change this. Swelling and congestion can block the way. This creates a strong sinusitis and sleep apnea link.
Normal Airflow Patterns During Sleep
At night, your body prefers to breathe through your nose. The nose keeps airflow steady and your throat muscles tight. Here’s how it works:
- Nasal passages warm and moisten air before it reaches your lungs.
- Smooth airflow reduces pressure changes that might collapse the throat.
- Natural filters reduce irritants that could trigger coughing or waking.
Sinus disease can disrupt the normal airflow through the nasal passages, leading to a narrowed airway and subsequent breathing difficulties during sleep.
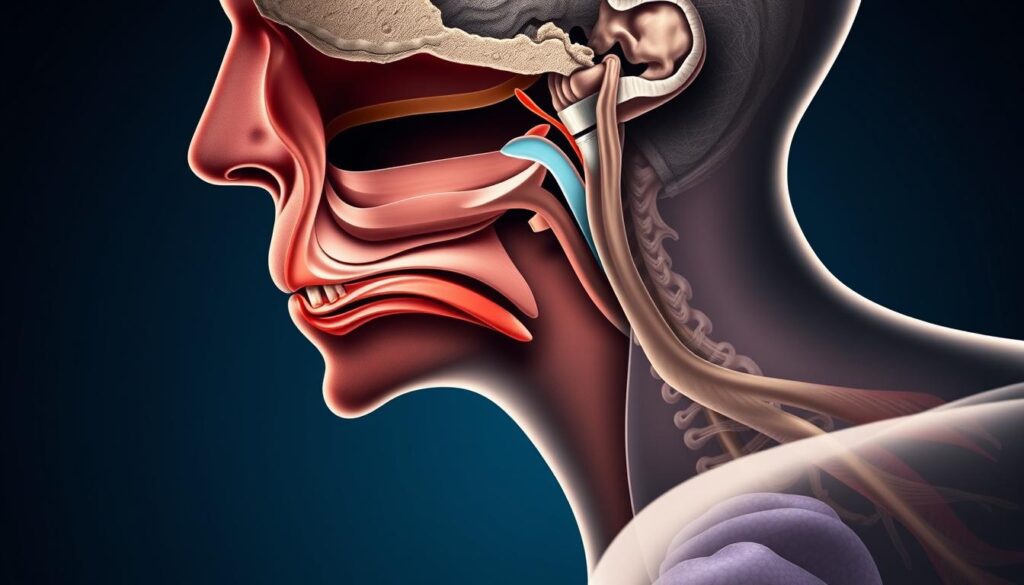
How Obstructions Impact Your Breathing
When sinusitis inflames tissues, you start breathing through your mouth. This makes your airway work harder. Here’s what happens:
Swollen sinuses → blocked nose → forced mouth breathing → increased airway resistance → higher risk of can sinusitis cause sleep apnea episodes. Mouth breathing can increase airway resistance by up to 250% compared to nasal breathing. This strain makes your throat muscles relax, causing blockages linked to sleep apnea.
Mouth breathing skips the nose’s natural protection. This leaves your throat open to collapsing at night. Knowing this can help you catch symptoms early.
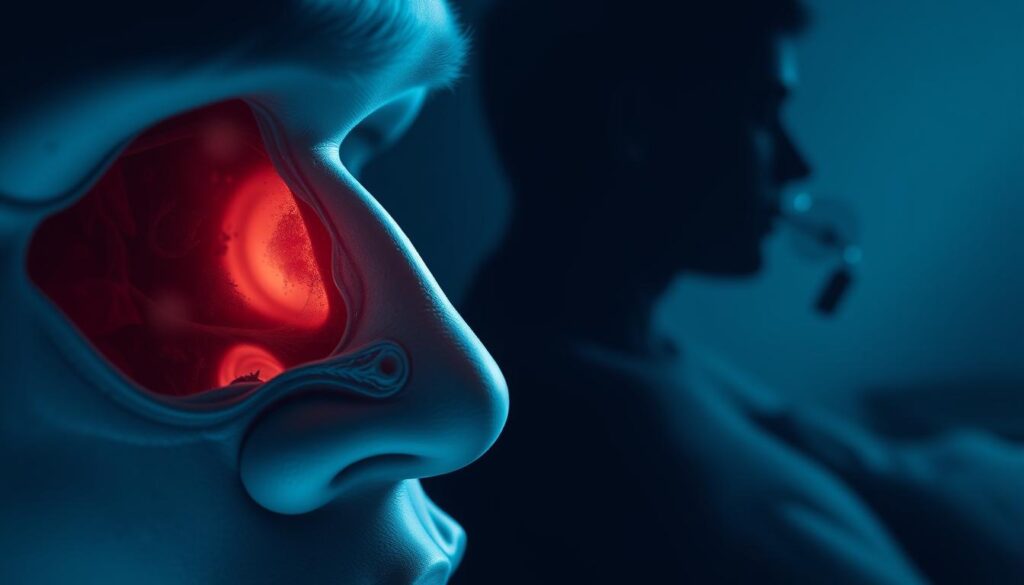
How Sinus Inflammation Contributes to Sleep-Disordered Breathing
Nasal congestion and sinus drainage are key in the sinus inflammation sleep apnea connection. Swollen nasal tissues from chronic sinusitis narrow airways. This makes breathing harder, lowering blood oxygen levels and disrupting sleep.
The relationship between sinusitis and sleep apnea also involves throat irritation. This irritation triggers muscle spasms that restrict airflow even more.
Nasal Congestion’s Impact on Oxygen Levels
- Chronic inflammation swells nasal passages, reducing airflow by up to 50%, per studies.
- Low oxygen levels during sleep can drop by 15-20% in severely blocked airways.
- A study found 64.1% of chronic sinusitis patients had clinically significant apnea (AHI >5).
Sinus Drainage and Throat Irritation
- Postnasal drip irritates throat tissues, causing inflammation and muscle spasms.
- 60% of CRS patients report worsened snoring due to throat swelling.
- Increased daytime sleepiness (Epworth Score >10) affects 38.1% of sinusitis sufferers.
| Sleep Symptom | Odds Ratio |
|---|---|
| Difficulty falling asleep | 3.98 |
| Snoring | 3.13 |
| Waking during the night | 3.44 |
| Early morning exhaustion | 4.71 |
| Daytime sleepiness | 4.56 |
These mechanisms create a cycle where sinus inflammation sleep apnea connection worsens both conditions. Using saline rinses or CPAP therapy can help. It improves airflow and sleep quality.
Signs That Your Sinusitis May Be Affecting Your Sleep
If you wake up often and have sinus problems, it might mean your sinusitis symptoms worsen sleep apnea. Look out for these signs:

- Waking with dry mouth or sore throat: Breathing through your mouth dries out your airways and causes irritation.
- Gasping or choking episodes: When your nose is blocked, you breathe less oxygen. This makes sleep apnea worse.
- Daytime fatigue despite 7-8 hours of sleep: Even without full apnea, partial blockages can break up your sleep.
- Observed pauses in breathing: Swollen sinuses make your airways narrower. This raises the risk of apnea during deep sleep.
- Chronic morning headaches: Not getting enough oxygen during blocked breathing can strain your blood vessels.
Research shows 70% of chronic sinusitis patients experience sleep disturbances linked to sinus issues and sleep apnea correlation, per recent studies.
Keeping a symptom diary can help doctors see the connection. For example, nasal drainage or worse snoring could mean the two conditions are linked. If you toss and turn a lot or your bed partner hears loud snoring, see a doctor. Untreated sleep issues can lead to serious problems like high blood pressure or brain fog.
See if over-the-counter sinus meds help you sleep better. If they do, it might show the sinus issues and sleep apnea correlation. Don’t ignore these signs. Treating both conditions together can lead to better results.
Diagnosing Both Conditions: What to Expect
Figuring out how sinus congestion impacts sleep apnea begins with tests. These tests show the sinusitis and sleep apnea link. Doctors use sleep studies and imaging to find the root cause. This ensures both conditions are properly diagnosed.
Sleep Studies and What They Reveal
Sleep studies track brain waves, breathing, and oxygen levels. They find when apnea happens. Home tests also watch breathing and blood oxygen.
A 2016 study found 7% of sleep apnea patients had sinusitis. This is compared to 2% of others. It shows a clear need for more investigation.
Sinus Examinations and Imaging
Doctors use CT scans and nasal endoscopies to see sinus blockages. A medical guideline says, “The best way to tell them apart is with a CT scan and a nasal endoscope.” These tools show inflammation or structural problems that disrupt sleep.
A 2015 study showed sinus surgery helped some sleep better. It proves imaging is key in treatment planning.
Questions Your Doctor Might Ask
- How long have you had nasal congestion or snoring?
- Do symptoms worsen at night?
- Have you tried over-the-counter treatments?
- Family history of sinus or sleep issues?
These questions help doctors figure out the sinus congestion impact on sleep apnea. The answers guide further steps like allergy tests or imaging.
Treatment Options for Sinusitis That May Improve Sleep Apnea
“Addressing sinus disease effectively can contribute to better management of snoring and sleep apnea.”
Many people with sinusitis find relief from sleep apnea symptoms when they treat their sinus issues. Sinusitis treatment for sleep apnea focuses on clearing nasal blockages. This helps you breathe through your nose instead of your mouth, which can stop snoring and improve sleep.
Let’s explore proven options:
- Nasal sprays: Corticosteroids like Flonase or Nasacort shrink swollen tissues, widening airways. They’re often paired with saline rinses to flush out mucus.
- Antibiotics: If bacteria cause your sinus infection, a 10-14 day course can reduce swelling, easing nighttime breathing.
- Procedures: Balloon sinus dilation gently expands blocked sinuses, improving airflow. This outpatient option works well for structural issues.
- Medication combos: Antihistamines or leukotriene inhibitors tackle allergy-driven congestion, while decongestants provide short-term relief.
When sinusitis improves, many see fewer apnea episodes. But if you still snore heavily or feel exhausted, additional steps may help. Losing even 10% of body weight can reduce sleep apnea severity, as obesity is a major risk factor. Sleeping on your side—using pillows to keep you positioned—also lowers snoring risk. For severe cases, CPAP machines deliver steady airflow, but addressing sinusitis first might reduce reliance on this device.
Always consult an ENT specialist to tailor your sinusitis treatment for sleep apnea. While sinus care can ease symptoms, it won’t cure all sleep apnea cases. Combining these steps with doctor-guided plans gives you the best chance for restful nights.
When Surgery Might Be Necessary for Both Conditions
When medicines and lifestyle changes don’t work, surgery might be needed. Surgery fixes problems that cause sinus and sleep apnea issues. Here’s what you need to know about surgery and how it works.
Ssinus Surgery Procedures
| Procedure | Purpose | Success Rate | Recovery Time |
|---|---|---|---|
| Functional Endoscopic Sinus Surgery (FESS) | Open blocked sinuses | 85-90% | 1–2 weeks |
| Balloon Sinuplasty | Expand sinus openings | 90% | 24 hours |
| Septoplasty | Correct deviated septums | 70-90% | 1–2 weeks |
| Turbinate Reduction | Shrink swollen tissues | 80% | 1–2 days |
Sleep Apnea Surgical Interventions
| Procedure | Purpose | Success Rate |
|---|---|---|
| Uvulopalatopharyngoplasty (UPPP) | Enlarges airway | 50-70% |
| Palatal Implants | Stabilize soft palate | Varies |
| Maxillommandibular Advancement | Realign jaws for severe cases | High for eligible patients |
Recovery and Expected Outcomes
Most sinus surgeries have quick recovery times. For example, balloon sinuplasty lets patients get back to normal in a day. FESS might need 1–2 weeks of rest.
Risks include infection or temporary loss of smell. Sleep apnea surgeries like UPPP take 2–4 weeks to heal. When surgeries treat both conditions together, success depends on the problem and following post-op care.
Lifestyle Changes to Manage Sinus Congestion and Sleep Apnea
Small changes in your daily habits can help. They can reduce how sinusitis symptoms worsen sleep apnea. By addressing the sinus inflammation sleep apnea connection, you can breathe better and sleep better. Let’s explore easy steps you can take at home.
“Sleeping on your back can worsen symptoms of both sinus congestion and sleep apnea. Elevatinging the head with pillows may help.”
Dietary Adjustments That Might Help
Eating foods that fight inflammation and avoid those that thicken mucus. Try these tips:
- Choose anti-inflammatory foods: Include turmeric, ginger, and omega-3 rich fish.
- Limit dairy, alcohol, and processed foods that can increase congestion.
- Stay hydrated with water to thin mucus and reduce sinus pressure.
Sleep Position Modifications
Adjust how you sleep to ease breathing. Side-sleeping keeps airways open and reduces snoring. Use a wedge pillow to elevate your head 4-6 inches. Avoid lying flat on your back, which traps mucus and narrows airways.
Environmental Controls for Better Breathing
Control your sleep environment to reduce triggers. Keep indoor humidity at 40-50% with a humidifier. Clean bedding weekly to remove dust mites and avoid allergens. Use HEPA filters to trap pollen and dander.
These changes work best with medical treatment. Talk to your doctor before making major lifestyle shifts.
When to Seek Immediate Medical Attention
If you have severe symptoms related to sinusitis and sleep apnea, get help fast. This can stop serious problems. Look for these warning signs:
- Having trouble breathing or feeling like you’re choking during sleep, even with treatments.
- A fever over 102°F (38.9°C) that lasts more than three days.
- Sudden vision changes, like seeing double or eye pain, which could mean the infection has spread.
- Severe headaches that don’t go away with pain relievers, especially near the eyes or forehead.
- Feeling confused, losing memory, or having sudden mood swings because of sleep problems.
- Facial swelling, especially around the eyes or cheeks, which is a sign of a serious problem.

Some symptoms need quick attention. For example, vision changes could mean the infection has reached your eyes or brain. Sinusitis symptoms worsen sleep apnea can also lead to brain problems, affecting your memory and mood.
If you have trouble breathing so much that it affects daily tasks like driving, get help right away.
Don’t wait if you have facial swelling, unexplained weight loss, or nosebleeds with sinus pain. These could mean you need surgery or special treatment. Tell your doctor if symptoms last longer than expected, like congestion over 12 weeks.
| Urgent Signs | Why It Matters |
|---|---|
| Sudden vision changes | Potential spread of infection |
| Memory loss or confusion | Linked to chronic sleep disruption |
| High fever + severe headache | Risk of meningitis or abscess |
It’s important to know when symptoms are serious. If you see red flags, call an ENT specialist or go to the emergency room. Quick action can prevent serious damage to your breathing or brain.
Conclusion: Taking Control of Your Sinus Health and Sleep Quality
Your health is linked to sinus issues and sleep apnea correlation. Over 70 million Americans face sleep problems due to chronic sinus issues. If you have trouble breathing at night or feel tired during the day, it’s a sign you need to act.
Getting a sinusitis treatment for sleep apnea starts with a doctor’s visit. Doctors might suggest nasal sprays, balloon sinuplasty, or CPAP machines. These can help clear your airways and improve your sleep.
Small changes can make a big difference. Try using saline sprays, stay away from allergens, and keep a good sleep routine. If problems continue, see a specialist for more help. Taking care of both conditions can boost your energy and lower heart disease risks.