Could that chest pain be from a sleep disorder you never thought of? The chest pain and sleep apnea connection is a big problem many ignore. When you stop breathing at night, your heart suffers a lot. Studies show up to 50% of sleep apnea patients feel chest pain, but most don’t link it to their sleep.
Can sleep apnea cause chest pain? Yes, it can. It happens because of low oxygen and stress hormones that hurt your heart.
Every night, sleep apnea makes your blood pressure go up and your heart work harder. This hidden effect means 80% of cases are missed, leaving symptoms like chest tightness without a clear cause. Even a little less sleep can increase heart risks. And 30% of chest pain patients might not get the right treatment. It’s crucial to understand this connection for your health.
Key Takeaways
- 30% higher risk of high blood pressure in those with sleep apnea.
- 2-3x higher heart attack risk compared to those without sleep apnea.
- 50% of sleep apnea patients report chest pain or pressure.
- 80% of sleep apnea cases remain undiagnosed, delaying treatment.
- Untreated sleep apnea doubles heart disease risk over time.
Understanding Sleep Apnea: What You Need to Know
Over 50 million Americans have sleep apnea, but many don’t know it. This condition makes breathing stop during sleep. It’s a silent battle your body fights every night.
Knowing about its types and effects helps you find warning signs early.
Types of Sleep Apnea: Obstructive, Central, and Complex
- Obstructive sleep apnea (OSA): Caused by blocked airways when throat muscles relax.
- Central sleep apnea (CSA): Brain signals fail, stopping breathing efforts.
- Complex sleep apnea: A mix of OSA and CSA, needing specialized treatment.
Common Symptoms of Sleep Apnea Beyond Snoring
Snoring is common, but other signs might surprise you. Look out for:
- Gasping or choking during sleep
- Morning headaches or dry mouth
- Daytime exhaustion despite “enough” sleep
- Irritability or memory issues
How Sleep Apnea Affects Your Entire Body
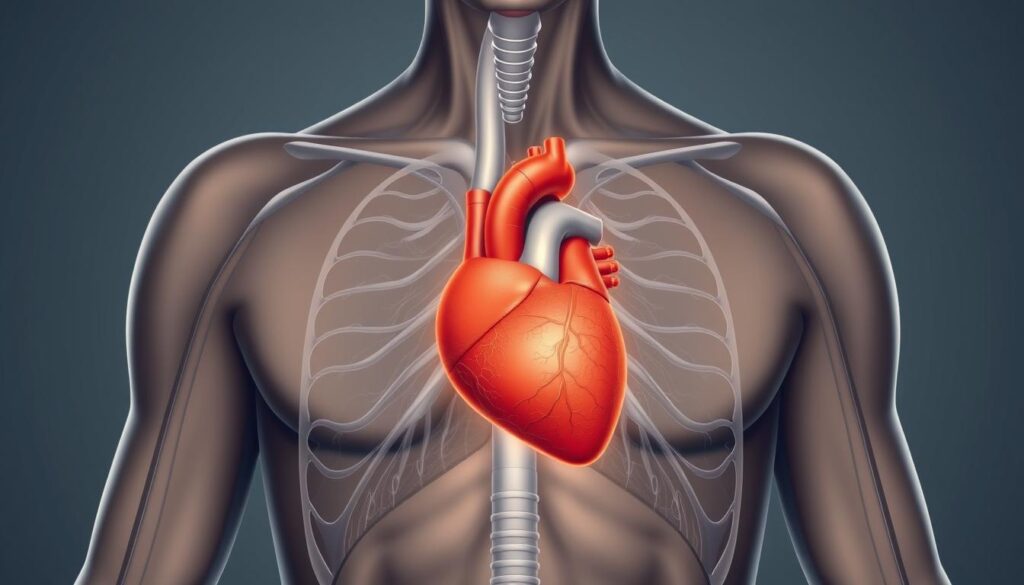
Each breath stop strains your heart and blood vessels. Sudden oxygen drops raise blood pressure and stress the cardiovascular system. This strain can lead to sleep apnea chest pain correlation through conditions like pulmonary hypertension.
Even your metabolic health suffers. This links to diabetes risk and weight gain. By understanding these connections, you can act before symptoms worsen. Early diagnosis stops silent damage, protecting both your sleep and long-term well-being.
Can Sleep Apnea Cause Chest Pain? The Direct Link
Yes, research shows can sleep apnea cause chest pain. Your heart goes through a lot during apnea. When you stop breathing, your blood oxygen drops and carbon dioxide goes up. This makes your brain wake you up to breathe again.
This cycle is hard on your heart. It can make your chest feel tight or pressured.
The Cardiovascular Strain During Apnea Episodes
Apnea events put sudden pressure on your chest. This makes your heart work harder. It raises your blood pressure and heart rate.
Studies by Cleveland Clinic say this can increase heart disease risk by 30%. It can also cause irregular heartbeats and strokes.
How Oxygen Deprivation Affects Your Heart
Low oxygen makes your heart pump harder. This can cause palpitations in 80% of people. It can also lead to chest pain during or after episodes.
 Low oxygen also stresses your arteries. This raises the risk of high blood pressure and heart attacks. Over time, it weakens your heart function, making symptoms worse.
Low oxygen also stresses your arteries. This raises the risk of high blood pressure and heart attacks. Over time, it weakens your heart function, making symptoms worse.
Distinguishing Sleep Apnea Chest Pain from Other Types
Sleep apnea chest pain is different from heart attacks or acid reflux. It feels like mild pressure or tightness during sleep. It may wake you up, unlike acid reflux’s burning.
Morning headaches or daytime fatigue with these symptoms mean you might have apnea, not digestive issues.
The Science Behind Sleep Apnea and Heart Health
Understanding chest pain from sleep apnea starts with its impact on your heart’s daily workload. Every time breathing stops, your body reacts as if under threat. Oxygen levels drop, triggering adrenaline surges that strain your heart. This cycle repeats hundreds of times nightly, stressing blood vessels and raising blood pressure.
“Individuals with sleep apnea face 4 times higher odds of atrial fibrillation, a dangerous irregular heartbeat,” notes the Sleep Heart Health Study.
| Risk Factor | Increased Risk |
|---|---|
| Heart Failure | 140% higher |
| Stroke | 60% higher |
| Coronary Heart Disease | 30% higher |
Over time, these stress responses create chronic inflammation and oxidative damage. Studies show CPAP therapy lowers blood pressure and reduces C-reactive protein, a marker of inflammation. Even small oxygen dips during sleep can damage arteries, making heart attacks more likely. For example, patients with severe sleep apnea (AHI ≥20) face 4.33x higher stroke risk than those without the condition.
- Low oxygen triggers adrenaline spikes, raising heart strain
- CPAP reduces heart risks by improving sleep and oxygen flow
- Metabolic syndrome (linked to 60% of sleep apnea cases) worsens cardiovascular damage
Protect your heart by addressing sleep apnea early. Even mild cases can silently erode heart health over years. Talk to a doctor if you wake up with chest tightness or irregular heartbeats—these are your body’s red flags.
Recognizing Sleep Apnea Chest Pain Symptoms
If you have chest pain from sleep apnea, it’s important to know the difference from heart problems. Many people feel morning chest tightness that gets better as the day goes on. This pain is usually not sharp like a heart attack.
- Morning symptoms: Pressure in the chest upon waking, easing by midday
- Nighttime episodes: Discomfort flaring during sleep, often paired with gasping or waking up
- Radiation pain: May spread to the neck, jaw, or arms but rarely the left arm
Nighttime sleep apnea chest pain symptoms often happen when you stop breathing. Watch if pain goes with choking or snoring. If pain gets worse when you lie flat, it might be obstructive sleep apnea.
Seek emergency care for:
– Severe crushing chest pain lasting >15 minutes
– Pain paired with cold sweats, dizziness, or arm/neck numbness
– Shortness of breath without obvious cause
More than 30% of OSA patients feel chest pain due to low oxygen at night. If symptoms don’t go away, see a doctor in 48 hours. Always treat sudden severe chest pain as urgent until it’s proven safe.
Diagnosing the Connection: Tests You Might Need
Figuring out if sleep apnea causes chest pain starts with tests. Your doctor will help you find out. They’ll check how breathing problems at night might hurt your heart.

At-Home Sleep Studies Simplify the Process
Most tests for sleep apnea chest discomfort start at home. You’ll wear a wrist monitor or small device. It tracks your breathing, heart rate, and oxygen levels all night.
These tests are easy and work for many people. If they show big breathing pauses, your doctor might want more tests. This could be an in-lab test that records brain waves and heart data.
Heart Tests Reveal the Full Picture
- ECG/EKG: Checks your heart rhythm for any problems.
- Echocardiogram: Uses sound waves to see your heart’s structure and how well it pumps.
- Stress Test: Watches your heart while you’re active to find hidden issues.
These tests help find heart problems from sleep apnea. Up to 80% of severe cases have heart strain. Finding it early can prevent high blood pressure or arrhythmias.
Questions That Matter
Doctors ask important questions to connect symptoms. They want to know when you feel chest pain and if it wakes you up. They also ask about snoring and your medical history.
Being honest about your sleep, medications, and lifestyle helps doctors. It makes finding the right treatment faster and more accurate.
Treatment Options to Relieve Sleep Apnea Chest Pressure
There are many ways to ease sleep apnea chest pressure. The main goal is to keep your airways open. This helps your heart and lungs feel better. Many people find quick relief with these methods:
- CPAP Therapy uses a mask to keep airways open. Most people feel better in just a few days. New machines are quieter and more comfortable.
- Oral Appliances like custom mouthguards help keep your throat open. They can cut AHI scores by over 50% in mild cases. This eases pressure over time.
- Positional Therapy devices stop you from sleeping on your back. This is the worst position for apnea. Using a wearable sensor or pillow can help.

For very bad cases, surgical options might be needed. The FDA-approved Remede System uses tech like a pacemaker to help breathing. Losing weight is also important: losing 10% of body weight can reduce AHI by 26%.
Using more than one method often works best. Your doctor might suggest nasal strips, acid reflux treatment, or oral exercises. Remember, sticking to therapy is key. Studies show CPAP use lowers heart risks long-term. Talk to your healthcare team today to find the right plan for your sleep apnea chest pressure.
Lifestyle Changes to Improve Both Sleep Apnea and Chest Discomfort
Small changes can make a big difference in reducing sleep apnea chest tightness and improving sleep quality. Here’s how to start feeling better tonight:

Weight Management Strategies
Even modest weight loss—like shedding 5-10% of your current weight—can ease airway pressure. Start with:
- Tracking meals using apps to avoid overeating
- Choosing protein-rich snacks to stay full longer
- Walking 30 minutes daily to boost metabolism
Sleep Position Adjustments
| Sleep Position | Impact |
|---|---|
| Back Sleeping | Worsens breathing and increases chest tightness |
| Side Sleeping | Reduces airway blockages and improves oxygen flow |
Try placing a pillow between your knees or a tennis ball sewn to your pajamas back to encourage side sleeping.
Diet and Exercise Recommendations
- Avoid alcohol and caffeine 3 hours before bed—they relax throat muscles
- Eat anti-inflammatory foods like ginger or turmeric to reduce airway swelling
- Do 10 minutes of throat exercises daily (e.g., tongue slides or singing)
Incorporate 150 minutes of weekly exercise like yoga, which boosts oxygen levels and strengthens respiratory muscles. Even small steps like swapping soda for water can make a difference.
Long-term Risks of Untreated Sleep Apnea and Chest Pain

Ignoring sleep apnea chest heaviness can cause serious health issues. Untreated apnea can harm your heart and lower your quality of life. It also raises the risk of other diseases. Here’s what happens if you delay getting help:
Potential Complications for Your Heart
Chronic sleep apnea chest heaviness often points to deeper problems. Studies show:
- Severe apnea (30+ breathing pauses/hour) raises heart attack risk by 200%.
- Untreated apnea doubles the likelihood of atrial fibrillation compared to those without the condition.
- Over 70% of coronary artery disease patients also have sleep apnea.
Impact on Overall Quality of Life
Living with untreated apnea can be tough. You might feel:
| Physical Effects | Chronic fatigue, headaches |
|---|---|
| Emotional Effects | Anxiety, memory fog |
| Everyday Challenges | Work accidents, relationship strain |
The Connection to Other Health Conditions
Sleep apnea doesn’t work alone. It can make other health problems worse or create new ones:
- Hypertension: 50% of OSA patients also have high blood pressure.
- Type 2 diabetes: Higher blood sugar spikes occur when you stop using your CPAP device.
- Immune system weakness: Chronic low oxygen weakens your body’s defenses.
Early treatment with CPAP can lower these risks. Research shows 70% of patients see blood pressure improvements within 3 months of consistent use. Don’t let chest discomfort become a lifelong health crisis.
Conclusion: Taking Control of Your Sleep and Heart Health
If you’ve wondered, ‘can sleep apnea cause chest pain,’ the answer is yes. Sleep apnea can hurt your heart and make it hard to breathe. But, you can do something about it.
Ignoring sleep apnea is not good. It can make your heart work too hard and increase blood pressure. Studies show many adults are at risk for sleep apnea, especially those with heart problems.
Getting help for sleep apnea is the first step. A doctor might suggest a sleep study or CPAP therapy. These can help lower blood pressure and reduce heart strain.
Changing your lifestyle can also help. Losing weight and sleeping in a better position can ease symptoms. These changes can improve your overall health.
Don’t ignore chest pain or tiredness during the day. Untreated sleep apnea can increase heart failure risk. But, early treatment can help.
If you’re feeling tightness in your chest or tired, see a doctor. Modern treatments like CPAP are now more comfortable. They can save lives.
By focusing on your sleep, you protect your heart and regain energy. Sleep and heart health are closely linked. It’s a chance to take control and live better.