Ever felt a knot in your stomach before a big decision? Or noticed your appetite vanish when stressed? Those gut feelings are real signals from your digestive system. It’s a network of organs and nerves working hard to keep you healthy.
Did you know your gut has over 100 million nerve cells? That’s more than your spinal cord. This system doesn’t just digest food. It also affects your mood, energy, and immune system.
For millions, digestive discomfort is a daily issue. Up to 40% of people face functional bowel issues. Many don’t know how gut health ties to mental well-being.
When your digestive system struggles, it can cloud your thoughts and drain your energy. It can even shape your emotional state. This journey will show how your digestive system talks to your brain, why gut microbes matter, and simple steps to improve your digestive health.
Key Takeaways
- Your digestive system contains over 100 million nerve cells, forming its own “second brain.”
- Functional bowel issues affect up to 40% of people, often linked to anxiety or depression.
- 90% of the body’s serotonin, a mood-regulating chemical, is produced in the gut.
- The vagus nerve acts as a bridge, sending signals between your gut and brain.
- Over 70% of your immune system resides in your gut, making digestive health foundational to overall wellness.
Understanding Your Digestive System: An Overview
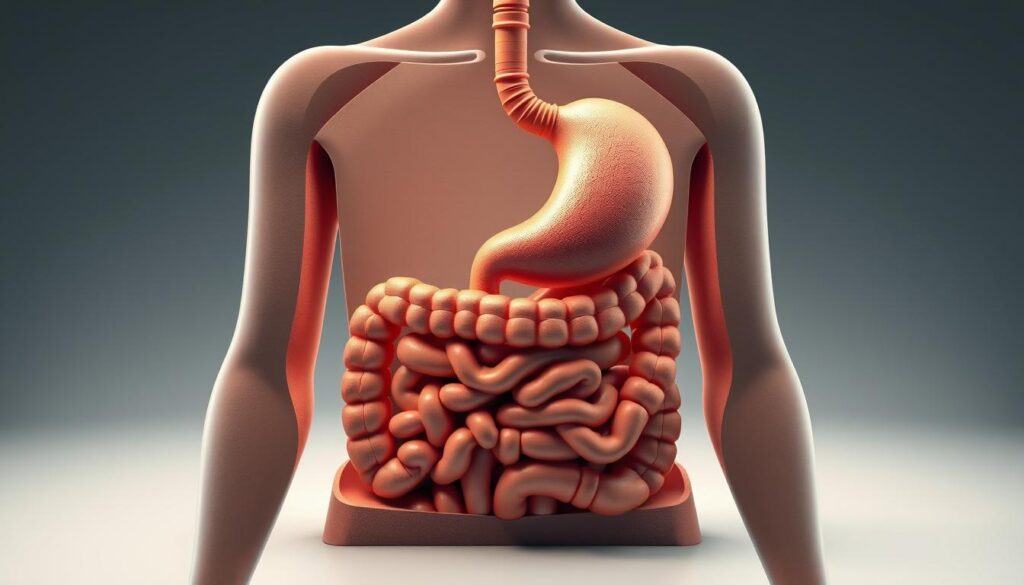
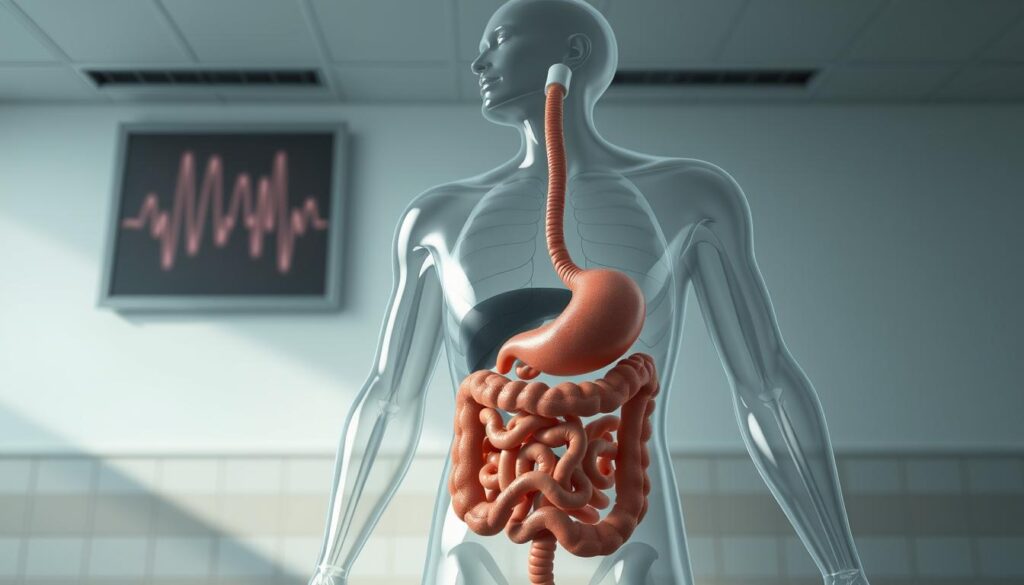
Your digestive tract is a key part of your body. It turns food into energy and nutrients. Let’s explore how it works.
What Makes Up Your Digestive System?
Eight main organs make up your digestive tract. These include the mouth, pharynx, esophagus, stomach, small intestine, large intestine, rectum, and anus. The liver, pancreas, and gallbladder also help digest food.
The small intestine is 20 feet long. It’s longer than your living room! This part of your body breaks down food, absorbs nutrients, and gets rid of waste.
The Journey of Food Through Your Body
- Food starts in your mouth, where chewing and saliva break it down.
- Then, peristalsis moves food into the stomach. The stomach mixes it into a liquid called chyme.
- The small intestine absorbs most nutrients. Tiny villi and microvilli help, with enzymes and bile from the pancreas and liver.
- Waste then goes to the large intestine. It pulls out water, making stool.
- Finally, waste leaves your body through the rectum and anus.
Why Digestive Health Matters
Ignoring your digestive system can cause problems. It can lead to bloating, fatigue, or serious issues. A healthy digestive tract has trillions of bacteria that help your immunity and make vitamins.
Even your mood is affected—70% of serotonin, which helps your mood, is made in your gut. When your digestive system is off, you feel it. Drinking water and eating foods high in fiber can help keep things running smoothly.
The Remarkable Journey: From Mouth to Stomach
Every bite you take starts a complex process. Your mouth is where digestion begins. Three major salivary glands make 1 to 1.5 liters of saliva daily. This saliva mixes with food to start breaking down carbs.
This liquid isn’t just wetness. Enzymes like amylase start breaking down nutrients before you swallow.
- Saliva softens food for easier swallowing.
- Enzymes in saliva begin digesting starches immediately.
Chewing well is not just polite—it’s science. The longer you chew, the more saliva mixes with food. This makes the journey ahead easier. 
Once swallowed, food goes through your throat. The epiglottis acts like a guard here. It closes over your windpipe during swallowing, preventing choking.
The esophagus then pushes food to your stomach with muscle waves (peristalsis). This happens in just 8 seconds. It shows how well your body’s systems work together for healthy digestion.
“Saliva is your body’s first tool for turning food into fuel,” says Dr. Emily Chen, a gastroenterology researcher. “It’s not just moisture—it’s a chemical powerhouse.”
Your stomach lining releases acids to break down food further. But the lower esophageal sphincter keeps acids in. Keeping this muscle strong prevents acid reflux.
Small steps like chewing well and staying hydrated help this process. They make digestion run smoothly.
The Small Intestine: Where Nutrient Absorption Happens
Your small intestine is a 20-foot powerhouse in your digestive system. It’s narrower than the large intestine. This coiled tube works hard to turn food into energy and nutrients your body needs. Let’s dive into how it does this job so efficiently.
The Three Sections of Your Small Intestine
- Duodenum (12 inches): Breaks down food with enzymes from the pancreas and bile from the liver.
- Jejunum (8 feet): Absorbs most carbs, proteins, and fats through its thin, permeable walls.
- Ileum (5 feet): Finishes absorbing vitamins like B12 and bile salts before sending waste to the large intestine.
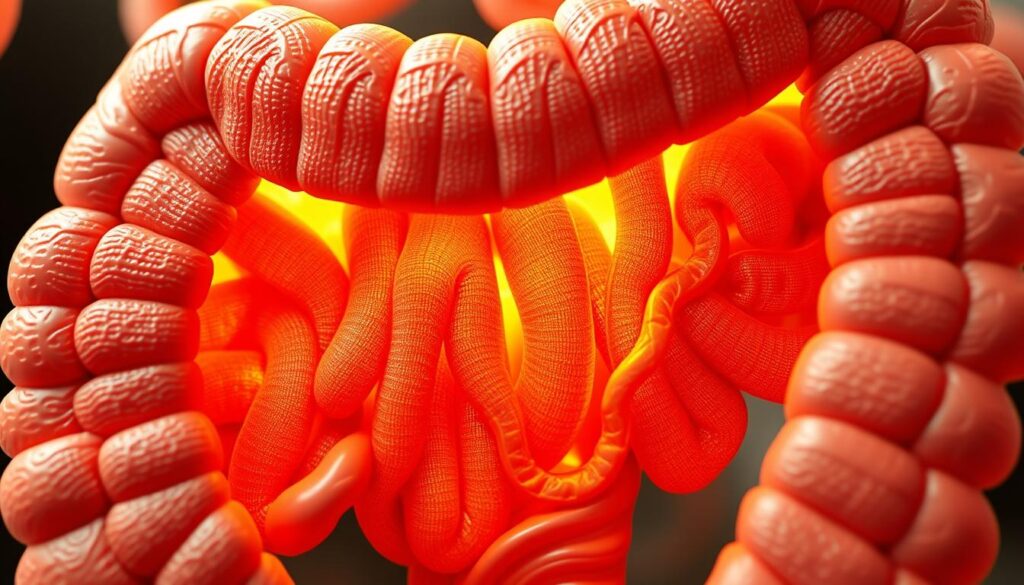
How Nutrients Enter Your Bloodstream
Imagine each nutrient as a passenger on a highway. Tiny finger-like villi and microscopic microvilli line your small intestine. They create a 600x larger surface area than flat tissue.
This lets nutrients like iron and vitamins slip through cells into your blood. Special carriers in cells grab vitamins and minerals. Water-soluble nutrients use channels to cross into blood vessels.
The Role of Villi and Microvilli
These tiny structures are like sponges! When damaged—like in celiac disease—nutrient absorption falters, harming gut health. Healthy villi ensure you get enough vitamins, minerals, and energy to fuel your body.
Without them, even a balanced diet might leave you deficient.
Your Large Intestine: The Final Processing Station
Think of your large intestine as the last stop in your digestive tract. It’s shorter than the small intestine, at about 5 feet long. Yet, it plays a big role in keeping your digestive health strong. It absorbs water, forms stool, and moves waste along.
It also hosts trillions of friendly bacteria. These bacteria help make vitamins like B12 and K.
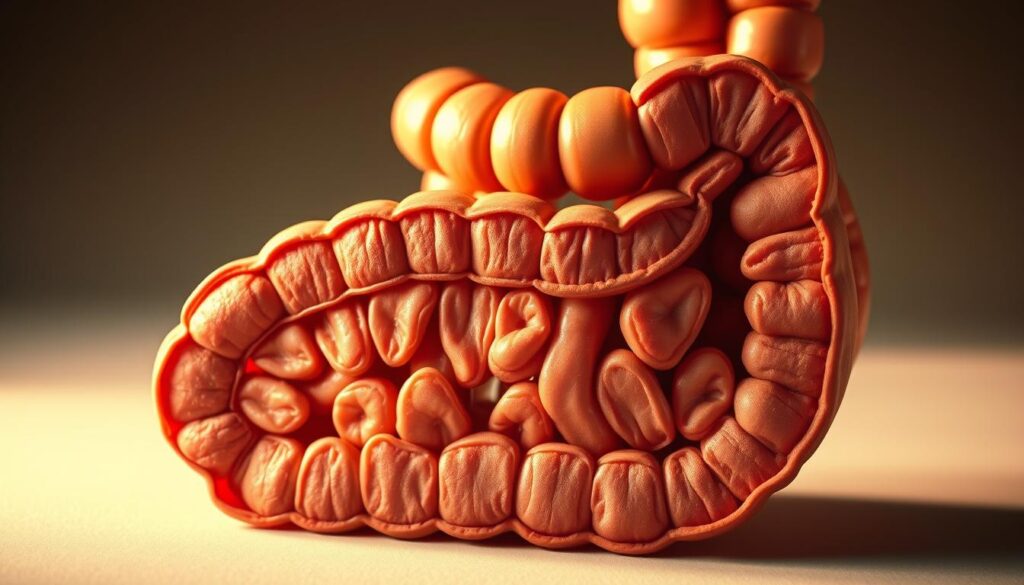
- Stores waste while removing up to 90% of remaining water
- Supports vitamin production through gut bacteria
- Contracts rhythmically to move material through its sections (cecum, colon, rectum)
Colon cancer screening saves lives: 30,000+ lives yearly are saved through early detection.
Listen to what your large intestine needs. Eating foods high in fiber helps prevent constipation. This affects 15% of Americans. It also keeps things moving well.
Drink plenty of water too. Dehydration can slow it down. Look out for signs like persistent bloating, blood in stool, or unexplained weight loss. These could mean problems like diverticulosis or IBS.
Keeping your large intestine balanced means caring for its microbiome. Probiotics in yogurt or fermented foods help its bacteria. And don’t forget regular check-ups starting at 45 (or earlier if there’s a family history). A healthy large intestine is key to your overall health.
Digestive Enzymes: The Chemical Heroes of Digestion
Your body needs digestive enzymes to turn food into nutrients. These proteins cut apart fats, carbs, and proteins. Without them, you might feel bloated or tired.
Types of Digestive Enzymes and Their Functions
Your pancreas makes 8 ounces of enzyme-rich juice every day. Here’s how they help:
- Amalyse: Starts breaking carbs in your mouth, finishes in your small intestine.
- Protease: Found in stomach acid, breaks proteins into amino acids.
- Lipase: Made by your pancreas, breaks fats into essential fatty acids.
When Enzyme Production Goes Wrong
Problems happen when your body can’t make enough enzymes. For example:
- 90% of cystic fibrosis patients need pancreatic enzyme replacement therapy (PERT) because of blocked pathways.
- Conditions like chronic pancreatitis or pancreatic cancer (95% start in enzyme-making cells) mess up production.
- As you get older, your body makes fewer enzymes, causing bloating or greasy stools.
Natural Ways to Support Enzyme Production
Help your body make more enzymes with these tips:
- Chew food well to activate amylase in saliva.
- Drink plenty of water to help enzymes dissolve food.
- Eat foods rich in enzymes like pineapple (bromelain) and papaya, but studies show little effect for most.
Supplements are available, but the FDA doesn’t regulate them. So, dosages vary a lot. Always talk to a doctor before taking them.
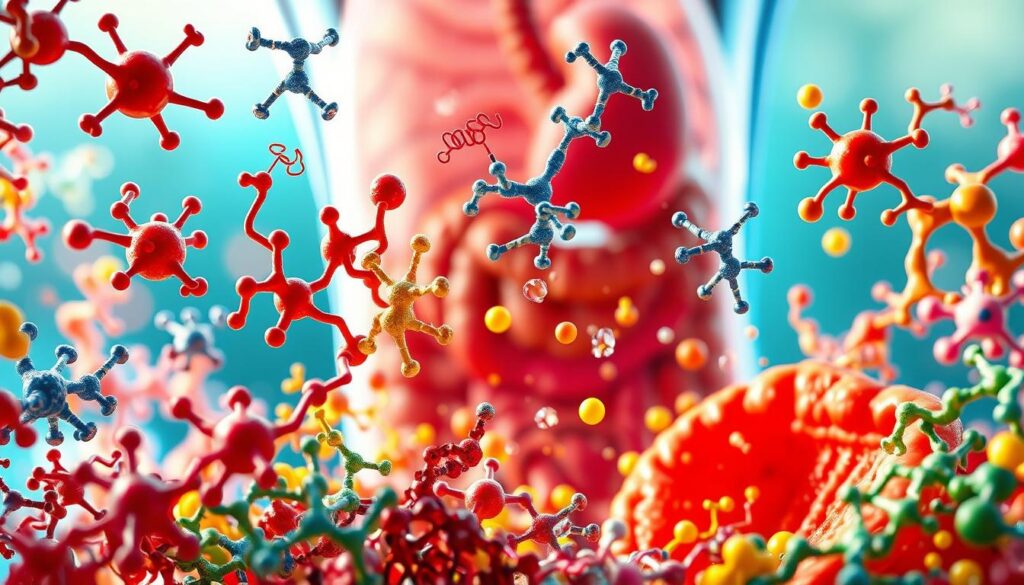
The Gut Microbiome: Your Digestive System’s Ecosystem
Trillions of microbes live in your gut. They form a community that affects your health. These tiny organisms help digest food and influence your mood and immunity.
How Gut Bacteria Influence Your Overall Health
Scientists found over 1,000 bacterial species in your gut. Each plays a role in your body’s functions. For example, some bacteria make serotonin, which makes you feel good.
An imbalance, called dysbiosis, can cause problems. It can lead to inflammation, weight gain, or heart disease. Gut microbes also affect how your body processes sugar and cholesterol.
“Breastfed babies have higher levels of Bifidobacteria, which supports immune development,” highlighting how early diet shapes lifelong gut health.
Building a Healthier Microbiome
Boosting your gut health starts with your diet. Try these strategies:
- Eat fiber-rich foods like oats, beans, and apples to feed beneficial bacteria.
- Include fermented foods (yogurt, sauerkraut) to introduce diverse microbes.
- Avoid artificial sweeteners—they can disrupt microbial balance.
Protect your digestive system by limiting antibiotics unless necessary. Prioritize sleep and stress relief. Chronic stress weakens microbial diversity. Plant-based diets rich in whole grains reduce harmful bacteria like E. coli, lowering inflammation.
Small changes today can lead to big rewards. Your gut microbiome isn’t just part of your body—it’s a partner in your health journey.
Common Digestive Disorders and Their Warning Signs
More than 60 million Americans deal with digestive problems every year. Spotting early signs can lead to timely treatment. Issues like irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and gastroesophageal reflux disease (GERD) are common.
- IBS: Bloating, cramps, constipation, or diarrhea. Affects 10–15% of adults, more often women.
- IBD (Crohn’s/colitis): Chronic inflammation, abdominal pain, bloody stools, weight loss.
- GERD: Chronic heartburn, acid reflux, and chest pain linked to lifestyle factors like diet.
- Celiac disease: Diarrhea, malnutrition from gluten intolerance. 83% of cases remain undiagnosed in the U.S.
“The gut-brain connection means digestive distress can affect your mood—and stress can worsen gut health. Emerging research shows gut inflammation may send signals to the brain, altering emotional states.”
Long-term issues like constipation or diarrhea might signal deeper problems. Signs like unexplained weight loss, blood in stool, or severe pain are serious. Early detection is key, like with colonoscopy for colon cancer, which has a 90% survival rate if caught early.
Pay attention to your body. If digestive problems last for weeks, see a doctor. Early treatment can prevent serious issues and improve your life.
The Connection Between Stress and Your Digestive Health
Stress and digestive health are closely linked. Your gut has its own nervous system, with more neurotransmitters than your brain. When you’re stressed, your body focuses on fight-or-flight, cutting off blood to your gut. This slows digestion and can cause bloating, cramps, or changes in bowel movements.

Stress doesn’t cause conditions like inflammatory bowel disease (IBD) but can make symptoms worse. When stressed, your gut may react physically, creating a cycle where digestive discomfort fuels more anxiety. Understanding this link helps you protect your gut health through proactive care.
How Your Gut Responds to Stress
During stress, your body stops “rest and digest” modes. This reduces enzyme production and slows gut movement. This can disrupt microbiome balance, leading to bloating, nausea, or irregularity.
Chronic stress may also trigger inflammatory responses, worsening conditions like IBS. The gut’s reaction isn’t just metaphorical—your “gut feelings” are real, rooted in this bidirectional brain-gut communication.
“Stress-induced digestive symptoms often reflect your gut’s sensitivity to emotional states,” notes research from the American College of Gastroenterology.
Stress Management Techniques for Better Digestion
Small changes can make a big difference. Try these science-backed methods to calm your gut:
- Diaphragmatic breathing: Slow, deep breaths activate the parasympathetic nervous system, easing tension.
- Mindful eating: Focus on meals without distractions to reduce stress during digestion.
- Regular exercise: Even a 20-minute walk daily can lower stress hormones and improve gut motility.
| Technique | Benefits for Digestion |
|---|---|
| Yoga | Reduces inflammation and improves gut blood flow |
| Meditation | Lowers cortisol, supportingin microbiome balance |
| Progressive muscle relaxation | Alleviates cramping and bloating caused by tension |
Combining these strategies builds resilience. If symptoms persist—like frequent heartburn or unexplained pain—consult a healthcare provider to rule out underlying issues. Small steps today can lead to better digestive health tomorrow.
Nutrition Tips for Optimal Gastrointestinal System Function
What you eat is key to a healthy gut. Exercise is also important. Studies show 150 minutes of activity a week can reduce gut inflammation. Mix these diet tips with exercise for better digestion.
Foods That Support Digestive Health

- Fiber-rich foods like spinach, quinoa, and chia seeds help move waste. Aim for 25–38 grams daily. Most people only get 10–15g.
- Choose probiotic foods: yogurt, sauerkraut, and kimchi boost gut bacteria. Strains like Bifidobacterium longum and Lactobacillus acidophilus ease IBS symptoms.
- Anti-inflammatory options like turmeric and ginger reduce gut inflammation. Omega-3s in salmon or walnuts also support colon health.
What to Avoid When Experiencing Digestive Issues
- Limit processed snacks and red meat—they can upset gut bacteria balance and increase artery-clogging compounds.
- Watch sugar alcohols: xylitol and erythritol in sugar-free products caused bloating in 60–70% of study participants.
- Cut back on alcohol and caffeine, which irritate the stomach lining. Track high-FODMAP foods like apples or onions if you have IBS.
Meal Timing and Digestive Wellness
- Drink water with meals to soften stool and prevent constipation. Hydration aids fiber to work effectively.
- Eat slowly—chewing thoroughly reduces gas. Stop eating 3–4 hours before bed to avoid nighttime reflux.
- Pair zinc-rich foods like nuts or oysters to meet your daily needs (8–11 mg). Deficiencies weaken gut lining protection.
Small changes can make a big difference in your gut health. Adjust these tips based on how your body responds. Remember, your gut health is unique!
When to See a Doctor About Digestive Concerns
Knowing when to seek help for digestive issues is important. If you notice certain symptoms, it’s key to see a specialist. Here’s what to watch for:
- Unexplained weight loss: Losing weight without trying could signal digestive disorders like inflammatory bowel disease or cancer.
- Blood in stool: Bright red or black, tarry stools may indicate bleeding from the GI tract. This requires urgent evaluation.
- Severe pain: Sudden sharp pain in the abdomen, especially lasting hours, might point to conditions like appendicitis or pancreatitis.
- Chronic symptoms: Heartburn more than twice a week, diarrhea lasting over two weeks, or constipation (fewer than three bowel movements weekly) need attention.

If symptoms like vomiting blood, jaundice, or difficulty swallowing occur, go to the ER. For persistent issues, schedule an appointment within two weeks. Gastroenterologists use tests like colonoscopies and endoscopies to diagnose problems early. For example, a colonoscopy every 10 years starting at age 45 is key for colorectal cancer screening.
Early detection saves lives. At Birmingham Gastroenterology, our experts specialize in diagnosing and treating digestive disorders, from IBS to celiac disease.
Don’t ignore warning signs like anemia symptoms (fatigue, weakness) or unintended weight loss. Gastroenterologists undergo years of specialized training to identify issues others might miss. If symptoms interfere with daily life, seek care promptly. Early treatment improves outcomes and prevents complications.
The Future of Digestive Health: Emerging Research and Treatments
Scientists are finding new ways to boost your digestive health every day. They’re making big strides in gut microbiome research and new treatments. Soon, you might get therapies made just for you or AI that finds colon problems early.

“The gut and brain are partners in health,” say experts. “Treatments targeting both systems may offer better relief for conditions like IBS.”
Recent studies show promising results:
- A new drug, mirikizumab, helped 28% of Crohn’s patients reach remission in trials—double the placebo group.
- Fecal microbiota transplants (FMT) now treat more than C. diff infections, with trials showing benefits for IBS and ulcerative colitis.
- AIs now detect polyps during colonoscopies, cutting unnecessary surgeries by 30%.
Researchers are also exploring ways to grow previously “uncultivable” gut microbes using tools like the iChip. This could reveal how these microbes affect your digestive system’s role in obesity, diabetes, and even mental health. The Human Microbiome Consortium’s work has already mapped key bacterial groups like Bacteroidetes, paving the way for personalized treatments.
With over 3,500 GI clinical trials now active, the future looks brighter. These innovations could help the millions living with daily digestive disruptions—and even save lives. Stay tuned as science continues rewriting the story of your gut’s potential.
Conclusion: Taking Charge of Your Digestive Wellness
Your digestive health is about diet, lifestyle, and knowing what’s going on inside you. Understanding your gut microbiome helps you absorb nutrients and fight off sickness. Start with a diet full of fiber from veggies and fruits.
These foods help soften and bulk up your stool. Drink plenty of water, eat small meals often, and cut down on processed foods. This keeps your gut bacteria healthy. Probiotics can also help with bloating or irregular bowel movements, especially after antibiotics.
Pay attention to how your body feels. Changes in bowel habits or pain are not normal. If you notice these issues, see a specialist like those at Austin Gastroenterology.
They can check for problems like C. diff or IBS early on. Regular health checks and tests are key to staying healthy.
Everyone’s digestive system is different. Manage stress with mindfulness or choose gluten-free if you’re sensitive. Focus on whole foods and staying hydrated. And don’t hesitate to ask for expert advice when you need it.
By taking care of your digestive health now, you’ll avoid discomfort later. You’ll build a strong foundation for your overall wellbeing.