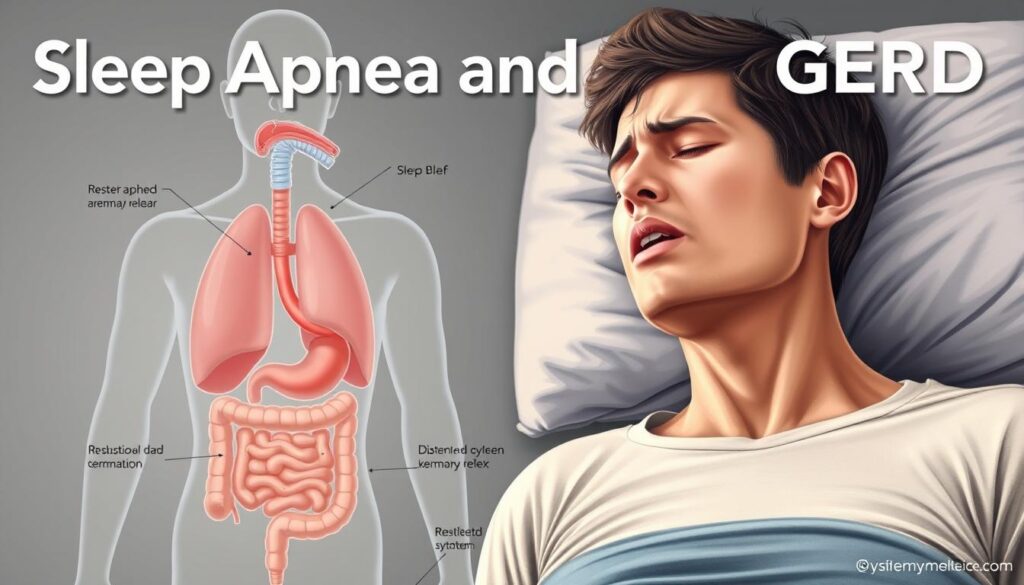
Ever wondered if sleep apnea and GERD are linked? The numbers are surprising. Over 12% of people with GERD also have sleep apnea. And the reverse is true too.
New research shows a clear link between sleep apnea and GERD. Could one condition trigger the other? Find out the facts about whether GERD is caused by sleep apnea and what it means for your health.
Millions of Americans face both conditions. For example, in GERD patients, nighttime symptoms are linked to sleep disturbances. But how do these two problems interact?
Learn why doctors now see a two-way street between apnea and GERD. Understanding this connection could change your treatment plan.
Key Takeaways
- 12% of GERD patients also have sleep apnea, per recent studies.
- Obesity raises your risk for both conditions—patients with GERD and OSA are 4x more likely to be obese.
- Over 80% of GERD symptoms strike at night, overlapping with sleep apnea’s impact on breathing.
- Diabetes and high blood pressure boost the chance of having both conditions.
- GERD and sleep apnea often share lifestyle risk factors you can address today.
Understanding Sleep Apnea and GERD: The Basics
Millions of Americans deal with sleep apnea and GERD. These two often go hand in hand. Knowing the basics can help you catch signs early.
What is Sleep Apnea?
Obstructive sleep apnea (OSA) happens when breathing stops during sleep. This is because throat muscles relax and block the airway. Signs include loud snoring, gasping for air, morning headaches, and feeling tired during the day.
Severe cases can happen over 30 times an hour. This can lead to heart disease and diabetes.
What is Gastroesophageal Reflux Disease (GERD)?
GERD is when stomach acid goes back up into the esophagus. Symptoms are heartburn, chest pain, and a sore throat. Over 20% of adults in the U.S. have GERD.
How Common is it to Have Both Conditions?
A 2022 study found a strong link between sleep apnea and GERD. 12% of GERD patients also had OSA, and 13% of OSA patients had GERD. This gerd and sleep apnea comorbidity gets worse with obesity or diabetes.
Knowing the symptoms of sleep apnea and GERD helps treat both better.
Does Sleep Apnea Cause GERD? Exploring the Connection
Doctors are still studying if does sleep apnea cause gerd. Current research shows a strong gerd and sleep apnea connection. During sleep apnea episodes, sudden pressure changes may pull stomach acid into the esophagus. This gerd caused by sleep apnea could explain why 60% of apnea patients also report GERD symptoms.
| Condition | Statistic |
|---|---|
| GERD weekly prevalence | 20% |
| Sleep apnea cases | 22 million in the US |
| Overlap | 60% of apnea patients have GERD |
Studies reveal intriguing links. For example, over 20% of Americans deal with weekly heartburn, and 22 million face sleep apnea. Of those with apnea, 60% also have GERD. Research in … shows…
Scientific studies highlight this relationship. A study in the American Journal of Gastroenterology found GERD patients were twice as likely to have sleep apnea symptoms. Meanwhile, gerd and sleep apnea connection studies show CPAP therapy reduces acid exposure by stabilizing breathing patterns. Some research even shows PPI medications improve sleep quality for dual sufferers.
- CPAP users report 25% less nighttime reflux
- GERD patients using PPIs see 40% better sleep outcomes
While the exact cause remains under study, the evidence shows a clear overlap. If you experience both issues, working with a specialist to address both conditions often leads to better results. Talk to your doctor about managing both to improve sleep and digestion.
The Physiological Link Between Sleep Apnea and GERD
Your body has natural ways to fight acid reflux. Sleep apnea can mess with these defenses. This messes up your body’s balance, making sleep apnea exacerbating gerd symptoms worse. The sleep apnea and gerd relationship is complex, with three main physical changes that make both conditions worse.
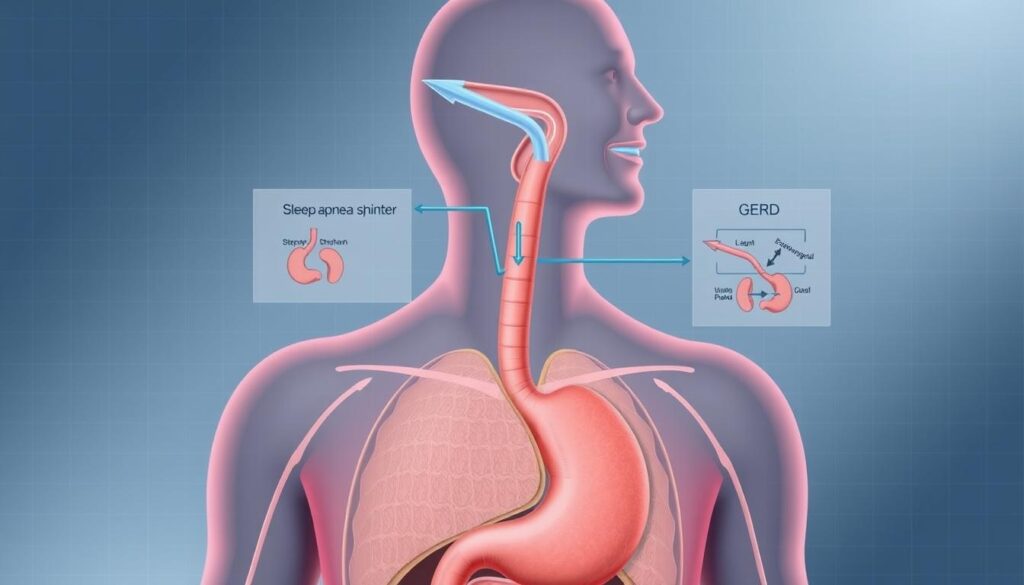
How Negative Pressure Changes Affect Your Esophagus
When you have sleep apnea, breathing is hard. This creates sudden drops in chest pressure. This drop pulls acid up into your esophagus, past the LES.
Studies show this is a big problem for GERD patients at night. Kim Y et al. found that worse OSA means more GERD damage seen during endoscopies.
The Role of Diaphragm Dysfunction
Your diaphragm helps keep acid down. But sleep apnea weakens it. This makes it easier for acid to get up.
A study by Leggett CL et al. found OSA increases the risk of Barrett’s esophagus. This shows how long-term damage can happen.
Why Sleep Position Matters for Both Conditions
Sleeping on your back puts more pressure on your stomach. This pushes acid up. Sleeping on your side helps a lot.
Studies show side sleeping cuts reflux episodes in half. This is good news for both sleep apnea and GERD.
| Factor | Impact | Study Reference |
|---|---|---|
| Negative Pressure | Increases LES opening by 40% during apnea | Cho YS et al. (2023) |
| Diaphragm Dysfunction | Raises hiatal hernia risk by 68% | Regenbogen E et al. (2022) |
| Back Sleeping | Linked to 5x more nighttime GERD episodes | Kim Y et al. (2021) |
Recognizing When You Have Both Conditions: Overlapping Symptoms
It’s important to know the symptoms of sleep apnea and gerd. Many people miss these signs because they seem unrelated. Here’s what to look out for.
Up to 4 out of 5 GERD patients face nighttime issues like acid reflux or coughing, per the International Foundation for Gastrointestinal Disorders.
Nighttime Symptoms to Watch For
- Gasping for air or choking during sleep
- Loud snoring paired with heartburn
- Waking with a sour taste or dry mouth
- Midnight coughing fits or chest discomfort
Daytime Signs That May Indicate Comorbidity
- Unexplained morning headaches or sore throat
- Persistent fatigue even after “rested” sleep
- Difficulty focusing or feeling mentally foggy
- Hoarseness lasting more than a few days
How to Track Your Symptoms Effectively
- Unexplained morning headaches or sore throat
- Persistent fatigue even after “rested” sleep
- Difficulty focusing or feeling mentally foggy
- Hoarseness lasting more than a few days
How to Track Your Symptoms Effectively
Keep a journal to track your symptoms. Use apps like SnoreLab for sleep or My GERD Diary for reflux. Note meals, sleep positions, and medications. Share this with your doctor to check for both conditions.
More than 50% of sleep apnea patients also have GERD. Yet, many miss this connection. Don’t ignore signs of both. Acting early can help your sleep and digestion.
The Bidirectional Relationship: How Each Condition Worsens the Other
The gerd and sleep apnea correlation makes both conditions worse. Sleep apnea pauses breathing, causing stomach acid to rise. This triggers sleep apnea exacerbating gerd.
GERD acid reflux at night disrupts sleep. This leads to more sleep apnea episodes. It’s a tough cycle for many to break.
Research shows 62% of sleep apnea patients also have GERD. This is nearly three times more than the general population. The main reasons for this are:
- Pressure changes during apnea episodes pulling stomach acid into the esophagus
- Acid exposure damaging throat tissues, making airway blockages more likely
- Chronic sleep deprivation reducing esophageal healing capacity
| Condition | Incidence per 10,000 (OSA) | Incidence per 10,000 (Non-OSA) |
|---|---|---|
| Barrett’s esophagus | 64.6 | 18.8 |
| Esophageal cancer | 7.4 | 3.9 |
| Esophageal stricture | 21.4 | 10.9 |
Untreated sleep apnea increases GERD risks. Patients with severe GERD symptoms have 3x worse sleep quality. Treating one condition alone often fails.
Both conditions share common risk factors like obesity (47.8% in dual-diagnosis patients) and metabolic issues. Using combined therapies, like CPAP for reflux control, improves outcomes. Breaking this cycle needs holistic care strategies.
Diagnosis Process: Getting Proper Testing for Both Conditions
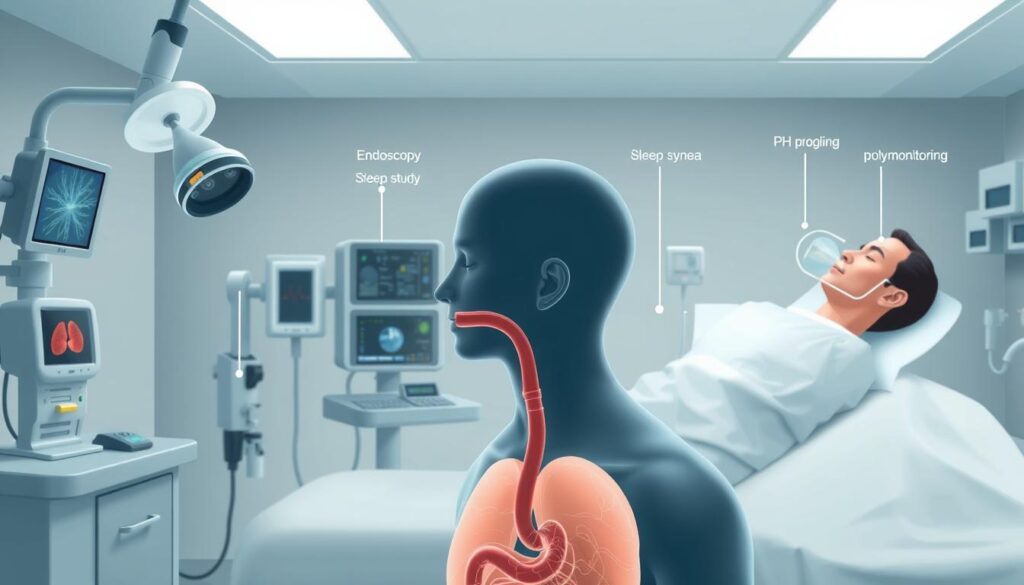
Understanding the gerd and sleep apnea connection starts with accurate testing. If you have chronic heartburn, snoring, or interrupted sleep, these steps help. They ensure you get the right care.
Sleep Studies Reveal Hidden Links
Sleep studies like polysomnography track your breathing and sleep patterns. Home sleep tests monitor apnea episodes. Over 58% of sleep apnea patients also have GERD.
Specialists look for symptoms like nighttime choking or frequent awakenings. Ask about overnight monitoring to spot the does sleep apnea cause gerd link in your case.
GERD Tests That Pinpoint the Cause
GERD evaluations include:
- Upper endoscopy to check esophageal damage
- 24-hour pH monitoring to track acid exposure
- Esophageal manometry for muscle function analysis
These tests uncover how reflux impacts your airways. Studies show 78% of sleep apnea patients report acid reflux. These tests are critical to ruling out gerd and sleep apnea connection causes.
Team Approach to Better Care
Work with a gastroenterologist and sleep specialist. Coordinated care improves outcomes: 75% of patients see symptom relief when both conditions are treated together. Bring a symptom diary to your appointments.
Note nighttime coughing, reflux episodes, and sleep disruptions. Ask for referrals to clinics experienced in managing both conditions.
Treatment Approaches When You Have Sleep Apnea and GERD
Managing sleep apnea and GERD together needs a special plan. GERD caused by sleep apnea often comes from breathing issues at night. Treating sleep apnea can help with acid reflux and breathing.
Research shows 38.9% of sleep apnea patients also have GERD. This makes it important to treat both conditions together.
CPAP Therapy and Its Effect on Reflux
CPAP machines, like those from Philips Respironics, keep airways open. This helps reduce GERD by lowering chest pressure. Some people find masks uncomfortable, but adjusting straps and using heated tubing can help.
Studies show CPAP therapy can lower reflux episodes at night. It keeps the airway pressure stable.
Medication Options for Managing GERD
Doctors often suggest:
- H2 blockers (e.g., famotidine) to cut acid production
- Proton pump inhibitors (e.g., omeprazole) for long-term acid control
- Antacids for quick heartburn relief
Always talk to your doctor to avoid bad reactions with other meds.
Positional Therapy Benefits
Using wedge pillows or adjustable beds to raise your head 6–8 inches helps. Sleeping on your side, especially the left side, also helps. A study found 65% of patients see better GERD symptoms with this therapy.

Combining these treatments makes a personalized plan. Treating sleep apnea can lessen GERD symptoms. GERD management can also improve breathing at night. Work with your team to find the right mix of treatments and check progress often.
Lifestyle Modifications That Help Both Sleep Apnea and GERD
Improving the gerd and sleep apnea correlation begins with daily choices. Making small changes can help your breathing, digestion, and sleep. Let’s look at effective ways to tackle both conditions.

- Watch your weight: Losing a little weight can help your airways and stomach. A 2022 study found that losing 5-10% of body weight helps many people.
- Sleep strategically: Use a wedge pillow or an adjustable bed to elevate your head. Sleeping on your left side can reduce acid exposure by up to 71%, studies show.
- Time meals wisely: Eat your last meal 3 hours before bed to avoid acid buildup. Stay away from acidic, spicy, or fatty foods at night.
- Move more: Regular exercise (30 mins/day) can improve sleep and digestion. But avoid hard workouts close to bedtime.
- Limit triggers: Drink less alcohol and stop smoking. Both can make sleep apnea worse and relax the esophageal sphincter, worsening GERD.
“Nighttime GERD symptoms are 3x more common than daytime issues, making sleep position adjustments critical.”
Small steps are important. Even small changes like raising your bed or eating lighter meals at night can help. Stick to these changes over time. They work with medical treatments to boost your health.
When to Seek Medical Attention for Worsening Symptoms
Knowing when to act is key in managing sleep apnea and GERD symptoms. Severe signs like chest pain or trouble swallowing need quick medical help. Since over 58% of sleep apnea patients also have GERD, it’s crucial to watch for red flags.
Warning Signs That Shouldn’t Be Ignored
- Sudden chest pain or choking during sleep
- Unexplained weight loss or blood in vomit
- Difficulty swallowing or chronic throat irritation
- Daytime drowsiness affecting work or driving
A study of 48 adults showed GERD can worsen sleep. If heartburn doesn’t get better with OTC meds, get help. Severe cases might need imaging or endoscopy to check esophageal damage.
Finding the Right Specialists for Your Care
Look for a gastroenterologist with GERD knowledge and a sleep specialist who knows about apnea. Ask if they treat both conditions. Academic medical centers often have teams for comorbidities.
“Sleeping at a 30-degree incline reduces reflux risk,” advises Dr. Allen, a leading ENT specialist.
Take a symptom journal to appointments to show when issues happen. Talk about any meds or CPAP therapy during consultations.
Conclusion: Managing the Sleep Apnea-GERD Connection for Better Health
Improving your health means tackling both gerd and sleep apnea. Studies show that treating one can help the other. For example, CPAP for sleep apnea cut GERD symptoms by 62% in users who followed the treatment.
Even small changes can help. Try raising your bedhead or avoiding late-night meals to reduce acid reflux.
Know your risk factors. Being female, overweight, or living in the southern U.S. increases your risk. Don’t ignore symptoms like nighttime choking or daytime fatigue. Work with doctors to track your sleep and acid reflux episodes.
Using treatments like CPAP correctly makes a big difference. Oral appliances might be a good option for those who find CPAP uncomfortable.
Every little bit helps. Losing a bit of weight can ease airway blockages and stomach acid pressure. Research shows treating sleep apnea can also reduce GERD episodes. Talk to your care team about how to tackle both conditions together. Small changes today can lead to better sleep and health tomorrow.