Did you know nearly 1 in 3 people with high blood pressure also have sleep apnea? The sleep apnea and high blood pressure connection is very strong. 30% to 40% of people with high blood pressure also have sleep apnea without knowing it.
This sleep disorder hypertension link is dangerous. It makes your blood pressure go up and stress hormones rise, even when you’re sleeping.
High blood pressure affects millions, but its link to sleep is often ignored. Healthy sleep should lower your blood pressure by 10-20% at night. This is called “dipping.”
But in severe sleep apnea, this doesn’t happen. Your body reacts to lack of oxygen with sudden heart rate jumps and stress hormone surges. This can make your daytime blood pressure too high.
OSA affects 24%-26% of men and 17%-28% of women aged 30-70. Many don’t know they have it because symptoms like loud snoring or gasping sounds are often ignored. But ignoring it is risky. Untreated apnea can make high blood pressure worse, strain the heart, and increase risks of stroke or heart attacks.
Key Takeaways
- Over 30% of hypertension patients also have obstructive sleep apnea, yet many remain unaware.
- Severe sleep apnea disrupts normal nighttime blood pressure drops, raising heart disease risks.
- CPAP therapy can reduce daytime and nighttime blood pressure in severe cases, but adherence rates remain low.
- Daytime BP rises with sleep apnea severity, worsening long-term cardiovascular health.
- Obesity, age, and lifestyle factors like poor diet tie both conditions together in a harmful loop.
Understanding Sleep Apnea and Its Prevalence
Obstructive sleep apnea (OSA) is a common sleep problem. It makes breathing stop many times during sleep. This is different from central sleep apnea, where the brain doesn’t tell the breathing muscles to work.
About half of OSA patients also have high blood pressure. And 30% of those with high blood pressure also have OSA.
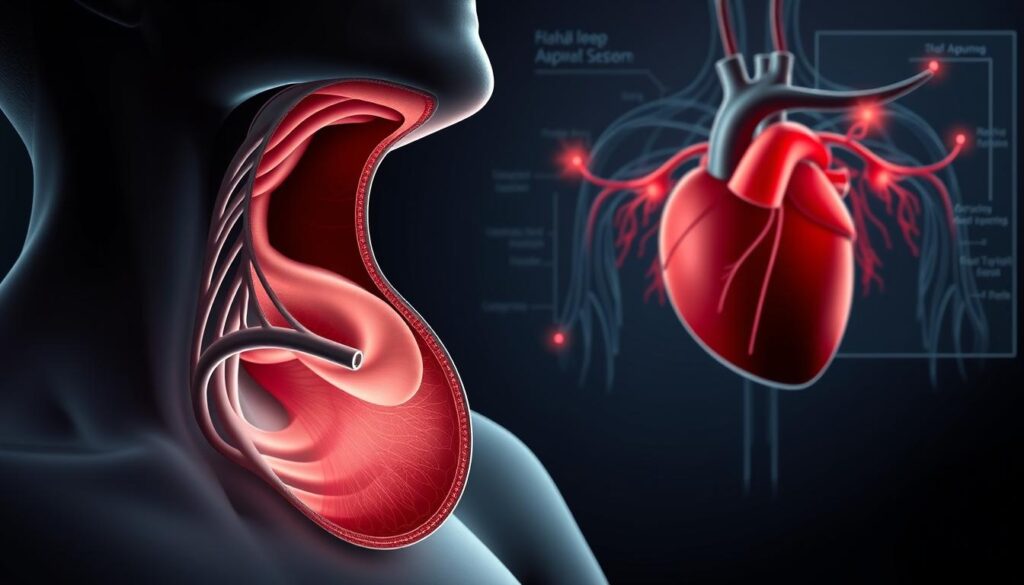
What Happens During Obstructive Sleep Apnea
When you have OSA, your airway closes off. This stops oxygen from getting in. It makes you wake up briefly, often without noticing.
These wake-ups hurt your heart and blood system. They make your blood pressure go up at night. Studies say it can go up by 15–19 mmHg.
Signs and Symptoms You Shouldn’t Ignore
- Loud snoring or gasping for air
- Morning headaches or dry mouth
- Daytime fatigue even after full sleep hours
- Difficulty concentrating or irritability
Risk Factors for Developing Sleep Apnea
Things that make you more likely to get OSA include:
- Excess weight or large neck circumference
- Male gender (2–4x higher risk than women)
- Aging, especially over 40
- Family history of sleep disorders
“The Wisconsin Sleep Cohort study confirmed that OSA increases long-term hypertension risk in a dose-dependent manner.”
About 30–40% of people with high blood pressure also have OSA. And 80% of middle-aged men with severe OSA don’t know they have it. Finding out early can stop heart problems and stroke.
The Sleep Apnea and High Blood Pressure Connection
Understanding the sleep apnea hypertension correlation starts with your body’s natural rhythms. When you sleep, healthy blood pressure drops 10–20%. But for those with obstructive sleep apnea (OSA), this drop doesn’t happen.
Instead, your body stays in high alert mode. This keeps blood pressure high all night. This relationship between OSA and high blood pressure creates a cycle that harms your heart.
| Condition | Nighttime Blood Pressure Dipping |
|---|---|
| Healthy Sleepers | 10–20% decrease |
| OSA Patients | Less than 10% decrease |
Research shows up to 50% of people with hypertension have OSA. This link grows stronger as OSA worsens. For instance, those with severe OSA face a higher chance of hypertension than those with mild cases.
Even morning blood pressure spikes matter—sudden rises upon waking raise cardiovascular risks.
Key stats to note:
- 71% of patients with hard-to treat high blood pressure have OSA
- Untreated OSA patients have 2x the risk of developing hypertension
If you’re managing high blood pressure, ask your doctor about sleep testing. Addressing OSA early can break this dangerous cycle and protect your long-term heart health.
How Nighttime Breathing Interruptions Raise Blood Pressure
Your body fights for oxygen and stress hormones at night. This battle harms your heart. The sleep apnea impact on blood pressure starts with each breathless moment. It sets off a chain of events that lasts long after bedtime.
When airflow stops, oxygen levels drop sharply. Your body responds by flooding your system with stress signals. Each apnea episode—lasting up to a minute—activates your “fight-or-flight” mode. This forces your heart to pump harder, raising BP with every interruption. Over time, this strain weakens blood vessel flexibility, making high BP more likely.
- Oxygen drops below 90% during apneas, activating stress pathways.
- Repeated oxygen crashes damage artery walls, increasing stiffness over months.
Each breathless pause triggers a flood of stress chemicals. Adrenaline and cortisol surge to juch you awake, but these hormones also cause BP spikes. For someone with severe OSA, this happens 10+ times every hour, keeping your BP elevated even after you wake up.
The effects don’t stop when you wake. Inflammation from nightly oxygen swings and ongoing stress hormone residue keep your BP high. Studies show 84% of OSA patients lose normal nighttime BP drops, leading to 24/7 strain. This OSa and hypertension relationship becomes a cycle that’s hard to break without treatment.
The effects don’t stop when you wake. Inflammation from nightly oxygen swings and ongoing stress hormone residue keep your BP high. Studies show 84% of OSA patients lose normal nighttime BP drops, leading to 24/7 strain. This OSa and hypertension relationship becomes a cycle that’s hard to break without treatment.
| Parameter | Normal Sleepers | OSA Patients |
|---|---|---|
| Nighttime BP Dipping | 10–20% reduction | No dipping; BP may rise |
| Stress Hormone Levels | Low during sleep | Elevated during apnea |
| Daytime BP | Returns to baseline | Often remains elevated |
“Untreated OSA’s 24-hour BP impact raises stroke risk by 50% in severe cases.”
Every breathless night adds to your heart’s workload. Breaking this cycle starts with recognizing the signs—and acting before damage becomes permanent.
Identifying Your Risk: When to Seek Medical Help

If you have high blood pressure and feel very tired, it’s time to look into sleep apnea cardiovascular risk. Many people with untreated OSA have a sleep disorder hypertension link that harms their heart. Here’s how to know if you should worry and what to do next.
Warning Signs of Sleep Apnea-Related Hypertension
- Daytime fatigue despite 7–8 hours of sleep
- Morning headaches or dry mouth
- Unexplained mood swings or anxiety
- Blood pressure that stays high despite medications
“Over 75% of patients with treatment-resistant hypertension also have sleep apnea,” says a 2022 study in the Journal of Clinical Hypertension.
Diagnostic Tests Your Doctor May Recommend
Your doctor might suggest overnight sleep studies (polysomnography) to track breathing and blood oxygen. Home sleep tests also measure air flow and oxygen. They’ll use 24-hour blood pressure monitors to check for nighttime spikes.
Don’t wait for symptoms to get worse. Early diagnosis can help reduce heart strain and improve blood pressure. If you or a partner notice gasping during sleep or frequent awakenings, talk to your doctor.
CPAP Therapy and Its Impact on Hypertension Management
CPAP therapy helps manage both sleep apnea and high blood pressure. It keeps your airway open at night. This can help stabilize your blood pressure.

A study by Usui et al. found that systolic BP decreased from 134.9 to 119.5 mm Hg with CPAP therapy. Diastolic BP also dropped from 75 to 65 mm Hg.
CPAP delivers steady air pressure through a mask. This prevents airway collapse. In a recent trial, 194 patients saw better daytime and nighttime blood pressure.
Those using CPAP 4+ hours nightly reduced their 24-hour BP by 4.4 mm Hg. It also cut nighttime riser patterns by 55% compared to no treatment.
- Average systolic BP dropped 4.9 mm Hg; diastolic fell 4.1 mm Hg
- 24-hour BP reached target levels in 18.4% of CPAP users vs. 13.8% without treatment
- Stopping CPAP use for just two weeks reversed blood pressure gains in many cases
Modern devices have adjustable masks and pressure settings. Over 70% of users adapt within a month. For best results, aim for at least 5 hours nightly use.
Pairing CPAP with lifestyle changes like exercise and diet maximizes blood pressure control.
Beyond CPAP: Additional Treatments for OSA and Hypertension
If CPAP doesn’t work for you, there are other ways to fight OSA and hypertension relationship. You can try lifestyle changes, medicines, and new gadgets. These options help manage both issues without a mask. Let’s look at what might work for you.

Lifestyle Modifications That Address Both Conditions
Small changes can make a big difference. Here are some tips:
- Weight loss: Losing 10% of body weight can cut AHI by 26%. It helps breathing and blood pressure.
- Exercise regularly: Doing 150 minutes of activity a week can lower BP and reduce OSA.
- Adjust sleep position: Sleeping on your side can cut AHI episodes by up to 50% compared to back-sleeping.
- Limit sodium and alcohol: High sodium diets can make both hypertension and OSA symptoms worse.
Medication Options for Managing Blood Pressure with Sleep Apnea
Doctors might change your hypertension meds to help with sleep apnea and high blood pressure connection. Here are some options:
- ACE inhibitors/ARBs: These drugs can lower BP and improve oxygen levels at night for some patients.
- Diuretics: Used carefully to reduce fluid retention without making apnea episodes worse.
- Customized schedules: Taking meds at bedtime can target nighttime BP spikes.
Alternative Therapies and Devices
Try these when CPAP isn’t an option:
| Treatment | Effectiveness | Key Benefit |
|---|---|---|
| Oral Appliances | 68% effective | Reduces AHI by 50%+ in most users |
| Positional Therapy | Halves back-sleeping AHI | Wearable devices prevent rolling onto back |
| Myofunctional Therapy | 50% AHI reduction | Exercises strengthen throat muscles |
| Bariatric Surgery | 86% OSA cure rate | Long-term weight loss improves both conditions |
Using different therapies together can work best. For example, using oral appliances with weight loss can lower BP by 5-7 points. Always talk to your doctor to find the right plan for your OSA and hypertension relationship.
Long-Term Health Risks of Untreated Sleep Apnea and Hypertension
Ignoring sleep apnea and hypertension can lead to severe long-term health consequences. The sleep apnea cardiovascular risk grows when breathing interruptions at night combine with high blood pressure. Over time, this sleep disorder hypertension link stresses your heart and blood vessels, increasing chances of life-threatening conditions.
- Heart Attacks and Strokes: Severe OSA raises heart attack and stroke risk by straining your cardiovascular system.
- Type 2 Diabetes: Poor sleep disrupts insulin sensitivity, worsening blood sugar control.
- Cognitive Decline: Chronic low oxygen levels can affect memory and focus over time.
- Chronic Kidney Disease: High blood pressure damages kidney blood vessels, impairing function.
| Risk Factor | Impact |
|---|---|
| Untreated OSA | 3x higher risk of fatal cardiovascular events |
| Severe Sleep Apnea | 60% increased stroke likelihood |
| Unmanaged Hypertension | 2x greater chance of heart failure |
If you delay treatment, your body faces compounding harm. Studies show 75% of those with treatment-resistant hypertension have undiagnosed OSA. Even small rises in blood pressure from sleep disruptions add up over years, accelerating artery damage. Early intervention with CPAP therapy or lifestyle changes can reduce these risks. Take action now to protect your heart, brain, and overall health before minor issues become irreversible.
Conclusion: Taking Control of Your Sleep and Heart Health
Your health is tied to good sleep and stable blood pressure. Sleep apnea can harm your blood pressure, leading to heart disease. The U.S. National Heart, Lung and Blood Institute says untreated sleep apnea can hurt your heart.
If you snore a lot or wake up gasping, see a doctor. CPAP therapy can help your breathing at night. It might also lower your blood pressure during the day.
Changing your lifestyle can also help. Losing weight, avoiding alcohol before bed, and exercising regularly can ease symptoms. Studies show treating sleep apnea can make your blood pressure better.
Obstructive sleep apnea and high blood pressure are connected but can be managed. Getting an early diagnosis is key. Focus on getting good sleep and following your treatment plan.
Small steps, like using CPAP or eating healthier, can make a big difference. Start taking care of your heart health today. It’s important to address these issues early and stay active in your health.