Could your snoring be a sign of a serious health condition affecting millions? Sleep apnea is a sleep disorder where breathing stops and starts during rest. The sleep apnea definition includes two main types: obstructive (OSA), caused by airway blockages) and central (CSA, linked to brain signaling issues). With 10-30% of U.S. adults affected, this condition often goes unnoticed.
Yet, untreated cases raise risks for heart disease, diabetes, and even sudden death.
Imagine waking up gasping for air dozens of times a night without knowing why. That’s daily life for millions. Over 30 million Americans live with sleep apnea, but 80% of severe cases go undiagnosed. This hidden disorder costs the U.S. over $149 billion yearly in lost productivity and healthcare.
Recent breakthroughs like FDA-approved Zepbound for OSA in 2024 offer hope—but first, you need to recognize the signs.
Key Takeaways
- 10-30% of U.S. adults have sleep apnea, yet 80% of severe cases remain undiagnosed.
- Obstructive sleep apnea (OSA) makes up 84% of all cases, often tied to obesity and anatomical factors.
- Zepbound became the first FDA-approved weight-loss drug for OSA in late 2024.
- Untreated sleep apnea doubles sudden death risk and raises diabetes chances by 30-50%.
- Annual economic costs exceed $149 billion due to untreated cases.
Understanding Sleep Apnea: A Common Yet Serious Sleep Disorder
What is sleep apnea? It’s when you stop breathing many times while sleeping. You might not even know it’s happening. Each time, you wake up a bit to breathe again.
These stops in breathing can make you feel tired, even after sleeping a lot. It’s because your sleep gets broken up.
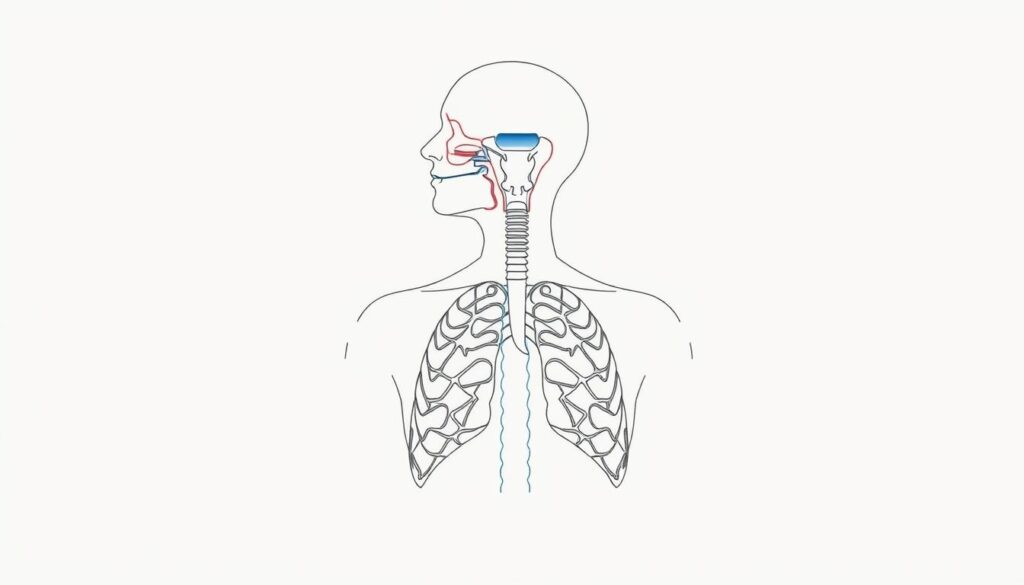
How Sleep Apnea Affects Your Breathing During Sleep
When you have sleep apnea, your throat muscles relax too much. This can block your airway. You might snore loudly or make choking sounds.
Your heart rate might slow down, and your blood oxygen levels could drop. These breathing pauses can harm your heart over time. They can also increase your risk of high blood pressure or heart disease.
The Prevalence of Sleep Apnea in the United States
- 10-30% of U.S. adults live with sleep apnea
- 30 million Americans have it, but only 6 million are diagnosed
- Men are 2-3x more likely than premenopausal women to be affected
Being overweight can also increase your risk. More than 20% of obese adults have sleep apnea. Age is another factor, with rates going up until the 60s.
Why Sleep Apnea Often Goes Undiagnosed
You might not hear the gasps or snorts because you’re asleep. Many people think tiredness is just stress or getting older. They might think it’s insomnia or anxiety instead.
Without someone to notice or a sleep study, it can go unnoticed for years. This quietly raises your health risks.
What is Sleep Apnea? Breaking Down the Definition
The sleep apnea definition is about breathing stops during sleep. What is sleep apnea? It’s when your airway blocks or collapses, causing breathing pauses or less airflow. These pauses must last 10 seconds and happen more than 5 times an hour.
| AHI Level | Episodes/Hour | Severity |
|---|---|---|
| Severe | >30 | Severe |
| Moderate | 15–30 | Moderate |
| Mild | 5–15 | Mild |
| Normal | <5 | Normal |
“Sleep apnea isn’t just loud snoring—it’s a hidden threat to your health,” say sleep experts. This condition affects 1 in 50 children and up to 90% of cases go undiagnosed. While snoringers may have it, not all snorers do. It’s also not limited to overweight individuals—genetics, anatomy, and health issues like thyroid problems also play roles.
- Myth: Only overweight people get it → Fact: Genetics and anatomy matter too.
- Myth: Snoring = sleep apnea → Fact: Snoring is a symptom, not a guarantee.
Understanding the sleep apnea definition means knowing it’s more than just interrupted sleep. It’s a medical issue needing attention to prevent long-term health risks like heart disease or strokes. If you’re waking up gasping or feel exhausted daily, talk to a doctor.
The Three Types of Sleep Apnea You Should Know
Learning what is sleep apnea means knowing its three types. Each type affects breathing in different ways. Understanding the causes and differences helps find the right treatment.

Obstructive Sleep Apnea (OSA): The Most Common Type
OSA happens when your throat muscles relax. This narrows your airway, causing snoring or gasping. Causes of sleep apnea include obesity, a large neck, or sleeping on your back. Over 84% of cases are OSA, making it the most common.
- Occurs in 10–30% of adults
- Linked to neck circumference and obesity
- Commonly treated with CPAP machines
Central Sleep Apnea: When Your Brain Misfires
This rare type occurs when your brain forgets to tell your body to breathe. Causes include heart failure, opioid use, or altitude sickness. Only about 0.4% of cases are this type.
- No airway blockage
- May require oxygen therapy or medications
- Risk rises with conditions like stroke or spinal injuries
Complex Sleep Apnea Syndrome: A Combination of Both
This rare form is a mix of OSA and CSA. Treatment often needs special CPAP modes. These address both airway blockage and brain signaling issues.
| Type | Cause | Prevalence |
|---|---|---|
| OSA | Physical airway blockage | 84% of cases |
| Central Sleep Apnea | Brain signal failure | 0.4% of cases |
| Complex Sleep Apnea | Mix of airway blockage and brain issues | 15% of cases |
Key Causes and Risk Factors of Sleep Apnea
Understanding the causes of sleep apnea can help you recognize personal risks. Let’s break down what science shows:

“Over 50% of people with obesity face a higher risk of sleep apnea due to excess neck fat compressing airways.”
Common causes include:
- Extra body weight: Fat around the neck or upper airway narrows breathing pathways.
- Physical traits like a thicker neck circumference (over 17” for men, 15” for women).
- Genetics: Family history plays a role, with 25-40% of cases showing hereditary links.
Key sleep apnea risks to watch for:
| Factor | Details |
|---|---|
| Age | Risk rises after 40, peaking in 60s-70s |
| Gender | Men are 2-4x more likely than women |
| Health habits | Smoking triples risk; alcohol relaxes throat muscles |
Modifiable risks like weight or smoking habits can be addressed. Non-modifiable factors like age or anatomy require proactive monitoring. Knowing these factors helps you take control of your sleep health.
Recognizing the Symptoms of Sleep Apnea
Spotting symptoms of sleep apnea early is key. It helps prevent health problems from getting worse. Over 60 million Americans struggle with sleep issues, many due to this condition. Knowing the signs can lead you to the right care.
Nighttime Symptoms You Might Notice
- Snoring so loudly it disrupts your partner’s sleep
- Gasping, choking, or silent breathing pauses
- Restless tossing and turning throughout the night
- Waking up with a dry mouth or headache
- Frequent nighttime trips to the bathroom
Daytime Signs That Could Indicate Sleep Apnea
- Feeling exhausted even after 7+ hours of sleep
- Morning headaches that persist past 9 AM
- Irritability or mood swings during the day
- Difficulty focusing on tasks or forgetfulness
- Unexplained drop in energy levels by afternoon
When to Seek Medical Attention
If these symptoms happen often, get a sleep apnea diagnosis. Look out for these red flags:
- Witnessed breathing pauses lasting 10+ seconds
- Daytime sleepiness that affects work or driving
- Chronic headaches with no other cause
- High blood pressure with sleep problems
Acting early can prevent heart disease. Don’t wait until symptoms affect your daily life. Protect your health now.
The Diagnostic Journey: How Sleep Apnea is Identified
Getting a sleep apnea diagnosis is the first step toward managing this condition. This process helps doctors confirm what is sleep apnea and its severity. Understanding the options available can ease concerns about testing.

Diagnostic methods vary based on your symptoms and medical history. Here’s a clear breakdown of your options:
Sleep Studies Explained
A polysomnogram (PSG) is the most accurate test. During this lab-based study, sensors track brain waves, breathing patterns, and oxygen levels. Doctors diagnose obstructive sleep apnea if you stop breathing five or more times per hour. Severe cases may reach 30+ events nightly.
At-Home Testing vs. Lab-Based Polysomnography
- Lab Studies: Offer detailed data on all sleep stages. Ideal for complex cases.
- Home Tests: Monitor airflow and oxygen levels. Best for people with clear risk factors like loud snoring or obesity.
What to Expect During Your Diagnosis Process
Start with a consultation where your doctor reviews symptoms like snoring or daytime fatigue. For a lab study, you’ll sleep overnight with sensors attached. Home tests use a simplified device worn overnight at home. Results usually arrive in 3–4 weeks, guiding your treatment plan.
Health Risks Associated with Untreated Sleep Apnea
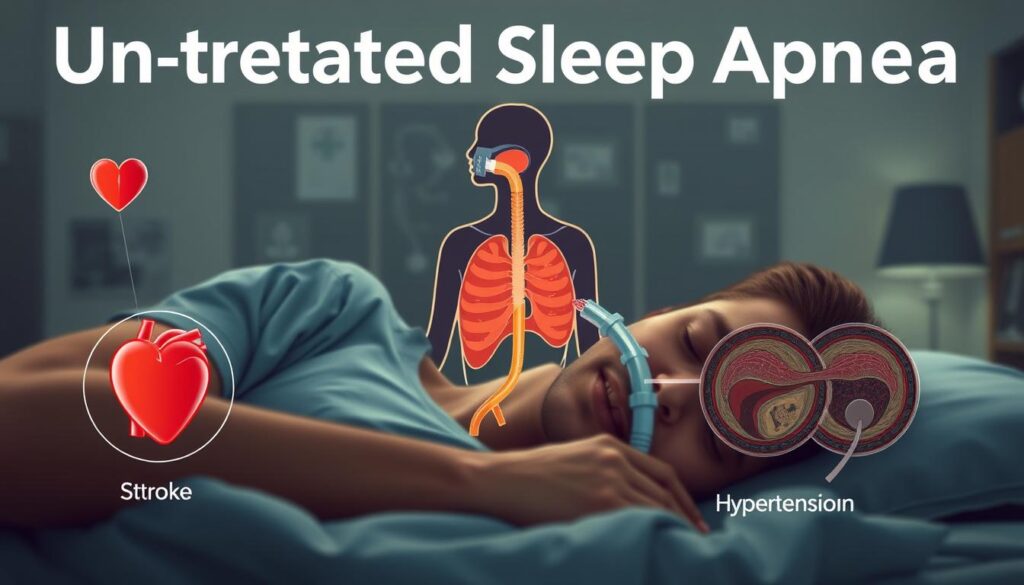
Untreated sleep apnea is very bad for your heart, brain, and health. Every day without treatment, your body gets stressed. This is because of low oxygen and broken sleep.
| Risk | Impact |
|---|---|
| Heart Disease | Double the risk of heart failure and strokes |
| High Blood Pressure | 50% of sleep apnea patients have hypertension |
| Car Crashes | 810,000 yearly accidents linked to drowsy driving |
| Diabetes | 37% of diabetics have severe sleep apnea |
- Stroke risk rises 3x in severe cases
- Memory problems and depression rates double
- Liver damage and fatty liver disease become more likely
Untreated sleep apnea costs the U.S. over $15 billion yearly in accidents alone.
Knowing what causes sleep apnea, like being overweight or having blocked noses, helps. But even without fixing every cause, treatment can help a lot. For example, CPAP machines can cut heart attack risk by 50%.
Ignoring sleep apnea risks is more than just feeling tired. It can lead to expensive and serious health problems. If you snore a lot or feel very tired every day, see a doctor. Early treatment can save your heart, money, and future.
Treatment Options for Managing Sleep Apnea
Choosing the right treatment for sleep apnea starts with knowing your diagnosis. Your doctor will help you find therapies that fit your needs. Good sleep apnea management often includes medical devices, lifestyle changes, and sometimes surgery.

CPAP Therapy: The Gold Standard Treatment
Continuous positive airway pressure (CPAP) devices help keep your airways open. Machines like CPAP, BiPAP, and APAP send steady air through a mask. Adjusting to these devices can take time.
Studies show CPAP makes you more alert. But, 1 in 3 people find the mask uncomfortable. New machines track how well you use them, helping doctors fine-tune settings.
Alternative Devices and Therapies
Oral appliances, like mandibular advancement devices, move your jaw to help breathing. For severe cases, implantable nerve stimulators (hypoglossal nerve stimulation) work during sleep. New devices like adaptive servo-ventilation (ASV) monitor breathing but are not safe for everyone.
Surgical Interventions for Sleep Apnea
- Uvulopalatopharyngoplasty: Removes throat tissue to widen airways.
- Radiofrequency ablation: Shrinks excess tissue with heat.
- Maxillomandibular advancement: Moves the jaw forward to open the airway.
- Tracheostomy: A last resort for life-threatening cases.
Surgeries may help but come with risks like scar tissue or nerve damage. Success depends on your body’s anatomy.
Lifestyle Modifications That Can Help
Small changes can make a big difference. Losing 20% of your body weight can reduce apnea episodes. Exercise for 30 minutes daily strengthens your throat muscles.
Sleeping on your side can prevent airway collapse. Avoid alcohol and sedatives before bed. They relax your throat muscles. In late 2024, the FDA approved Zepbound, a weight loss drug for treating moderate-severe OSA in obese patients.
Living Well with Sleep Apnea: Daily Management Strategies
Managing sleep apnea is more than just using medical devices. Simple daily habits can greatly help. Clean your CPAP machine every day and change filters monthly. When you travel, take your CPAP in a portable case and check airline rules for medical items. Being consistent is crucial for living with sleep apnea.

“Talk to any doctor—primary care, dentist, or therapist—for support. Sleep apnea affects overall health, so a team approach works best.”
Here are some daily tips to better your sleep:
- Stick to a bedtime routine: Go to bed and wake up at the same time every day.
- Limit alcohol 3-4 hours before bed to prevent airway relaxation.
- Exercise regularly—aim for 150 minutes of aerobic activity weekly.
- Use a humidifier to ease dryness from CPAP use.
Positional therapy is also helpful. Use a wedge pillow or positional trainer to sleep on your side. Avoid sleeping flat on your back to reduce breathing pauses. If stress or anxiety come up, think about joining a support group or counseling. Keep a journal to track symptoms and share with your care team.
Make your sleep area calm. Keep it cool, dark, and quiet. Also, change your mattress every 5-8 years for better spinal support. These small steps help build a routine for long-term sleep apnea management.
Sleep Apnea in Special Populations

Children, pregnant people, and older adults face special challenges with sleep apnea. Spotting symptoms early can stop serious problems. Let’s look at how it affects these groups in different ways.
Children and Sleep Apnea: What Parents Should Know
In kids, what is sleep apnea often comes from big tonsils or adenoids, not just being overweight. Watch for signs like bedwetting, being too active, or breathing pauses. A tonsillectomy might help many kids. Finding out early can stop delays in growth or learning.
Sleep Apnea During Pregnancy
Pregnancy makes sleep apnea risks higher because of weight gain and hormone changes. If not treated, it could lead to high blood pressure or early birth. Doctors might change CPAP settings to fit your body changes. Always talk to your healthcare team for advice that fits you.
Aging and Sleep Apnea: Changes Over Time
As we get older, our body changes and health issues like heart disease make symptoms worse. Older adults might sleep less well, leading to tiredness during the day. Getting a CPAP that fits you and treating other health problems is important for managing symptoms.
| Group | Risk Factors | Common Symptoms | Recommended Actions |
|---|---|---|---|
| Children | Enlarged tonsils | Behavioral issues | Surgery, monitoring growth |
| Pregnant Women | Hormonal shifts | Snoring, morning headaches | CPAP adjustments |
| Elderly | Neck circumference, comorbidities | Daytime sleepiness | Regular screenings, device adjustments |
Preventive Measures: Reducing Your Risk of Sleep Apnea
Knowing symptoms of sleep apnea early is key. Simple changes can help. Let’s look at steps you can take today.

Weight Management and Sleep Apnea Prevention
Being overweight can narrow airways. Almost 50% of obese people have sleep apnea. Losing 10% of your weight can help.
- Eat more fruits, veggies, and lean proteins.
- Do 150 minutes of aerobic exercise each week.
Sleep Position and Its Impact on Breathing
Most sleep apnea sufferers sleep on their backs. This can block airways. Try:
- Use a body pillow to sleep on your side.
- Try anti-snore shirts or devices to stay on your side.
Avoiding Substances That Worsen Symptoms
Alcohol and sedatives can make breathing harder. Smoking also increases risk. Limit these to protect your sleep:
- Don’t drink alcohol 3 hours before bed.
- Ask your doctor for sedative alternatives.
“Small changes in lifestyle can make a big difference in managing sleep apnea,” says the American Academy of Sleep Medicine. “Focus on consistency, not perfection.”
By making these changes, you can sleep better and avoid health risks. Talk to your doctor to make a plan that’s right for you.
Conclusion: Taking Control of Your Sleep Health
Living with sleep apnea doesn’t have to control your life. It affects over 1 billion people worldwide. If you notice loud snoring, gasping, or feeling tired during the day, act now.
Understanding your risks and getting a diagnosis is key. Many people, especially those who are overweight or older, are at risk. Yet, over 425 million adults worldwide have it and many don’t know.
There are effective treatments like CPAP therapy and lifestyle changes. Even small steps, like losing weight or sleeping on your side, can help. These steps can lower your risk of heart disease and accidents.
Your sleep health is important. Talk to your doctor today. A simple test could be your first step to better sleep. After a good night’s sleep, you should feel full of energy.
Don’t let sleep apnea hold you back. Take control of your well-being and enjoy restful sleep.